“Now I can walk for miles!”: Improving Access to Podiatry for Homeless People in Tower Hamlets
25th June 2024
Authors: Eleanor Mata (Therapy Manager), Stephanie Benjamin (Clinical Lead Podiatrist) and Clarissa Sørlie (Improvement Advisor)
The Tower Hamlets Foot Health team are using quality improvement to improve access to their services for homeless people to ensure timely care for foot related issues, prevent complications and promote mobility and comfort.
According to Tower Hamlets Council (2024), 624 people presented as homeless (or at risk of homelessness) in Tower Hamlets between April and June 2023. It is estimated that up to two thirds of homeless people experience foot problems yet only a quarter of those access healthcare (Mullins et al., 2022). Homeless people are at increased risk of injury to their feet, are likely walk longer distances, and are less likely to have access to clean socks and properly fitting shoes (To et al., 2016). For people with high-risk conditions such as diabetes and reduced sensation, poor adherence to treatment can contribute to worsening foot health. Stephanie Benjamin, clinical lead podiatrist, reflected, “There was a gap in foot health provision for this client group, particularly in the E1 area of the borough where services seek to support this client group through GP and housing services. The client group are often transient, not linked to primary care systems, and have a tendency toward a shorter life span.”
Figure 1. Left to right: Stephanie Benjamin (Clinical Lead Podiatrist), Marielle Fidele (Principal Information Analyst), Eleanor Mata (Therapy Manager) and Muniba Ali (Specialist Homelessness Podiatrist)
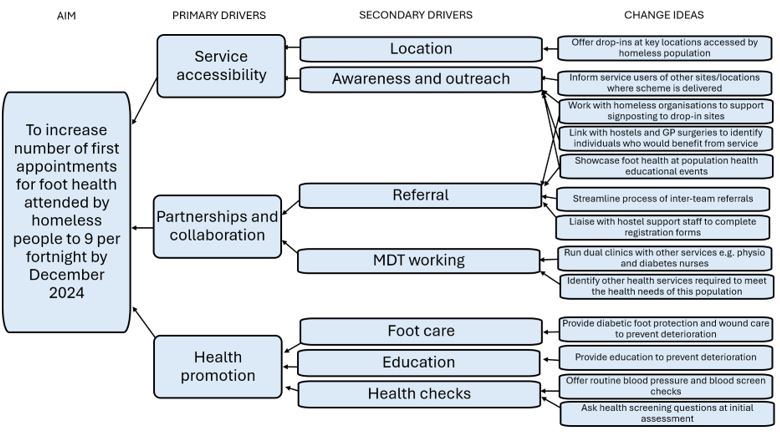
Recognising that homeless people were under-represented in their service, the community podiatry team in Tower Hamlets decided to start a quality improvement project. They set out to provide early identification and intervention of foot health disorders (such as trench foot, chilblains, blisters and frostbite), and prevent further deterioration, thereby reducing the need for people to access primary and secondary care services, particularly for vascular intervention and amputations/limb loss. The team also saw an opportunity for early identification of other health problems and making earlier referrals to other care pathways. They captured their theory of change using a tool called a driver diagram (see Figure 2).
Figure 2. Driver diagram illustrating the team’s theory of change
The team started offering regular drop-in appointments at locations already accessed by homeless people, as well as proactive visits to homeless hostels across the borough. Through these interactions, the team aspired to improve individuals’ confidence and knowledge of how to safely and independently manage their foot health care, and when/how to seek help.
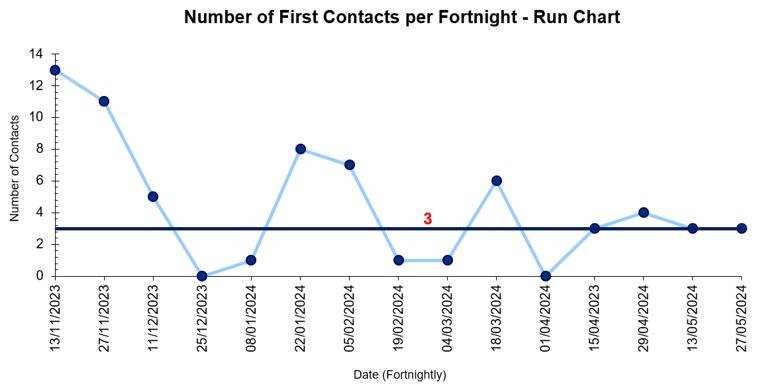
The team are now recording an average of 3 first appointments per fortnight (see Figure 3), with 88 homeless people on their caseload. An average of 6 people are returning per fortnight for follow-up appointments.
Figure 3. Run chart showing the number of first contacts per fortnight
Now that the team are successfully delivering tailored care to homeless people, they are learning how to maximise attendance at their clinics, and how to document service users’ treatment on electronic care records without a named GP or fixed address. They are also testing out ways of working more closely with hostels and other homeless organisations to support signposting and registration.
The team are collecting feedback from service users to understand the impact of their efforts. One service user remarked, “before I came to the clinic I couldn’t walk very well. Now I can walk for miles!”
Figure 4. A service user receiving treatment in a foot health clinic
A special thank you to Stephanie Benjamin, whose passion for improving equity for this population has been pivotal to getting this project off the ground. Stephanie is retiring from the Trust at the end of this month, but the team will continue to work through her change ideas which are documented on the driver diagram.
References:
Mullins, R.M., Mannix, R.E., Marshall, N.J. and Lewis, V.J. (2022) ‘Responding to Foot Health Needs of People Experiencing Homelessness: the Role of a Publicly Funded Community-Based Podiatry Service’, Journal of Foot and Ankle Research, 15(15). DOI: 10.1186/s13047-022-00518-7
To, M.J., Brothers, T.D., and Van Zoost, C. (2016) ‘Foot Conditions Among Homeless Persons: A Systematic Review’, PLoS One, 11(12). DOI: 10.1371/journal.pone.0167463
Tower Hamlets Council (2024) ‘Residents’ Views Sought on Homelessness’. (Accessed: 5th June 2024)
Most Read Stories
-
Why is Quality Control important?
18th July 2018

-
2016 QI Conference Poster Presentations
22nd March 2016
-
Recognising Racism: Using QI to Help Take Action
21st January 2021

-
QI Essentials: What does a Chief Quality Officer do?
18th March 2019

-
Using data enabled us to understand our problem
31st March 2023

-
The Power of Data in Reducing Pressure Ulcers
12th January 2022

Follow QI on social media
To keep up to date on the latest concerning QI at ELFT, follow us on our socials.