
The challenge of breaking barriers – OCEAN equity project learning and persevering
8th November 2024

Pic 1- Bedfordshire & Luton OCEAN Service
The Challenge?
Women and birthing people from Black, Asian and other minority ethnic backgrounds are at increased risk of experiencing adverse events during pregnancy and childbirth. This shows up as tokophobia in their subsequent pregnancies. Tokophobia places them and their babies at increased risk of further adverse events, unless support can be provided. However, referrals to Bedfordshire & Luton Ocean for women and birthing people from these backgrounds does not reflect the local population.
The service was receiving an average of 5 tokophobia referrals a month for people of BAME background from the Luton area; around 30% of all Luton tokophobia referrals. Not reflective of the social make-up of the area.
The Aim?
To increase identification and support of moderate to severe tokophobia in birthing people from Black, Asian and other minority ethnic backgrounds by increasing tokophobia referrals from the Luton area to Ocean by 25% by October 2024
But first… what is Tokophobia?
Tokophobia is an intense fear of pregnancy and childbirth. This condition can cause significant anxiety and distress, leading some individuals to avoid becoming pregnant or to opt for a Caesarean section to avoid vaginal birth.
There are two types of tokophobia:
- Primary tokophobia: This occurs in individuals who have never given birth. It may begin during adolescence or after becoming pregnant for the first time.
- Secondary tokophobia: This develops after a traumatic childbirth experience, miscarriage, stillbirth, or other pregnancy-related trauma.
Symptoms can include sleep disturbances, panic attacks, nightmares, and avoidance behaviours.
What is OCEAN?
OCEAN (Offering Compassionate Emotional Support for those Living Through Birth Trauma & Birth Loss) is an integrated maternity and mental health service providing support for those affected by birth loss or birth trauma.
The service is provided by East London NHS Foundation Trust (ELFT) in partnership with Bedford Hospitals NHS Foundation Trust.
The OCEAN Service provides:
- Specialist psychological treatment, care and support to those experiencing or those who have experienced a birth trauma and/or loss
- Targeted assessment/intervention for individuals identified with moderate/complex mental health needs arising from, or related to their maternity experience
- Therapeutic care that integrates psychological support, specialist midwifery support, and support around reproductive health.
It provides support for individuals experiencing moderate to severe mental health needs arising from:
- Birth trauma
- Pregnancy loss (due to miscarriage, stillbirth, or termination for any reason)
- Neonatal death
- Parent infant separation following birth due to safeguarding concerns
- Severe fear of childbirth
The aim is to provide joined-up care across mental health, maternity and reproductive health. This will fill in the gap where there is no other suitable existing service.
On To The Project…
The team of psychologists, managers, service users, and midwives started this project in 2023, led by Principal Clinical Psychologist, Dr. Amanda Spong. The project was part of our ELFT pursuing equity programme.
Combining their lived expertise and clinical knowledge, they broke the issue down into 3 primary drivers: Reducing stigma, Increasing knowledge and awareness, and Number of referrals.
With the support of people participation, the team got to work co-producing an information leaflet, outlining what tokophobia is, and information about what the OCEAN service has to offer. This leaflet was designed to have approachable, easy to understand language. They predicted this would help increase awareness of the service, contributing to increasing access to the target groups.
Whilst collecting data to back up this theory, design began on another, more ambitious, change idea: A joint OCEAN/Obstetric clinic at Luton & Dunstable (L&D) Hospital.
The vision of this was:
- To run a clinic jointly staffed by an Ocean specialist midwife and a consultant obstetrician at L&D hospital.
- To create referral pathways from community and hospital midwifery for women accessing routine antenatal care, bringing trauma-informed assessment and support into universal midwifery services.
- To test if this increases awareness or reduces stigma about accessing specialist support when previous loss or trauma is impacting the mental health and perinatal wellbeing of pregnant women and their unborn child.
Dr. Amrita Viegas and Karen Cook-Smith set up this clinic to run on Monday mornings at the L&D hospital antenatal service.
The standard operating procedure for the clinic was written and reviewed by the QI project team, then submitted and approved through Luton and Dunstable governance channels.
In January 2024, doors opened for the first PDSA cycle of testing.
The Results So Far…
The team embraced QI methodology of learning from our system with data. The results were interesting. Not all predictions were fully met, but all tests brought new learning.
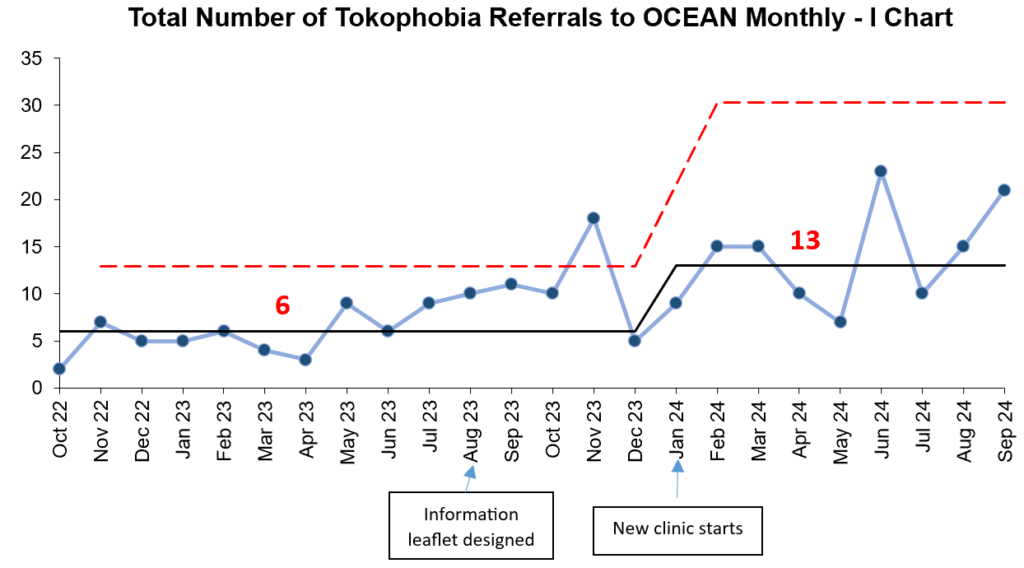
The team has over doubled their monthly tokophobia referrals! However, it is important to note that this data covers all ethnicities – not just BAME. It’s clear access has improved as a whole, but the real sign of success is seeing increases in the target group specifically…
Which we have!
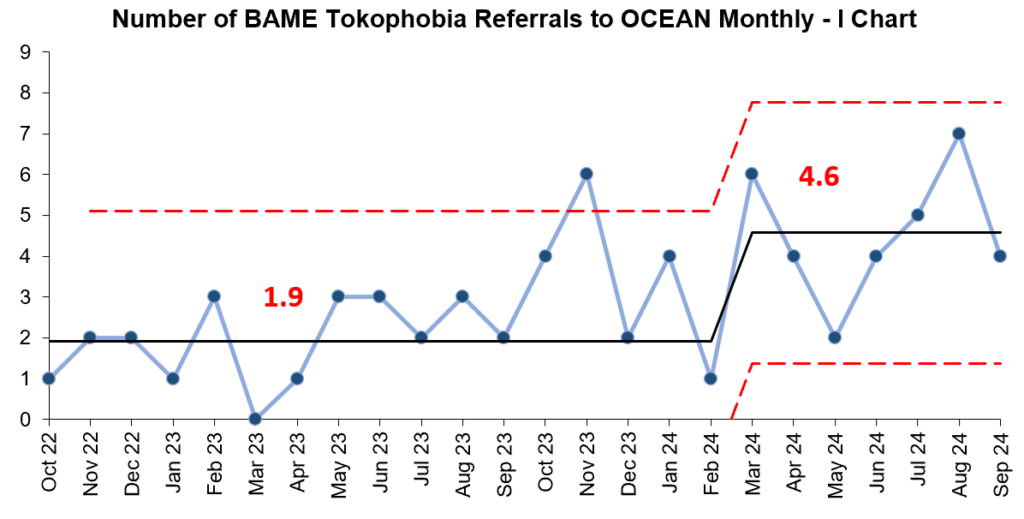
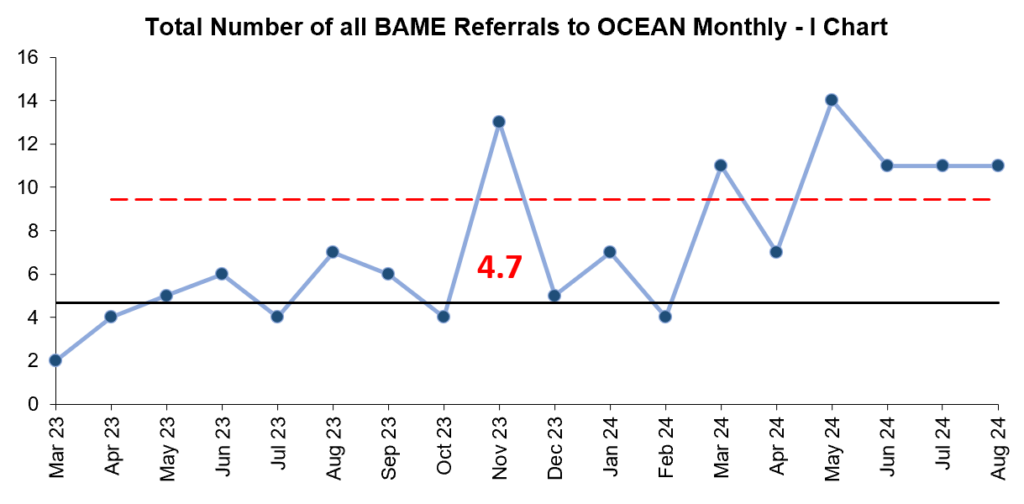
The charts below are showing an increase in the count of both BAME tokophobia referrals to OCEAN and promising signs of improvement in the number of total BAME referrals (not just tokophobia).
Not Finished Yet!
Whilst these numbers are encouraging, the team predicted greater gains. When looking at these numbers as a percentage of all referrals, the proportion remains the same. Access has increased… but it’s increased for everyone – has the equity gap really been closed?
The team regrouped to discuss this conundrum. They concluded that they need to be more targeted in their approach. They’ve evidenced that the new clinic does provide effective care, but the true barriers of access lay a stage before it. Whilst the clinic continues its testing, Karen Cook-Smith, Emotional Wellbeing Midwife, is gathering more data and service user/ carer stories to help refine its delivery.
The next chapter of the project journey must go outside the organisation, deeper into the community. The first demographic of focus is Pakistani Urdu speaking women.
The Next Change Idea
- Identify facilitators and barriers to Urdu speaking women accessing specialist support for tokophobia.
- Increase referrals to Ocean from Urdu speaking women for tokophobia support and treatment.
- Translate coproduced tokophobia leaflet into Urdu.
- Speak to leaders of mosques in East Luton to ask permission to distribute leaflet and/or speak to women in their community about tokophobia and support available
The project team is fortunate to be able to tap into their Urdu speaking expertise to plan this next PDSA cycle. With lived experience at the heart of this project’s success, this also involves the creation of a new Urdu speaking Pakistani service user focus group, to steer the next cycle with lived expertise.
Watch this space. They’re not finished yet.
Most Read Stories
-
Why is Quality Control important?
18th July 2018

-
An Illustrated Guide to Quality Improvement
20th May 2019

-
2016 QI Conference Poster Presentations
22nd March 2016
-
Recognising Racism: Using QI to Help Take Action
21st January 2021

-
Using data enabled us to understand our problem
31st March 2023

-
QI Essentials: What does a Chief Quality Officer do?
18th March 2019


Follow QI on social media
To keep up to date on the latest concerning QI at ELFT, follow us on our socials.


