Addressing the under-representation of patient groups accessing the Tower Hamlets Psychological Therapies Team
8th November 2024
Written By Vahishta Pardiwalla (Senior Counselling Psychologist) with contributions from Dalila Magdu (Tower Hamlets Quality Improvement & Governance Coordinator and Vernanda Julien (Improvement Advisor)

Figure 1: Tower Hamlets Psychological Therapies Team
The Psychological Therapies Service (PTS) in Tower Hamlets identified a significant under-representation of the people accessing the service, which prompted the need for a Quality Improvement (QI) project aimed at enhancing access and inclusivity. To tackle this problem, a project team was formed, consisting of psychologists, administrative staff, assistant psychologists, trainee psychologists and experts by experience.
Baseline data revealed that certain groups—such as men, older adults, and individuals of Bangladeshi heritage—were not accessing services in proportion to the local population.
When the project began in 2022, only 16.08% of PTS clients identified as Bangladeshi, compared to 34.6% in the local population. Only 30.8% of clients were male despite making up 50.21% of the borough’s population. Additionally, both younger adults (18-19) and older adults (60+) were underrepresented, while individuals aged 20-34 were over-represented.
Alongside this quantitative data, feedback from service users underscored issues of accessibility and inclusivity, highlighting that some clients felt underrepresented within the service. To explore these themes further, qualitative research was conducted through trainee-led projects. These included a focus group study investigating men’s experiences in accessing the service and an in-depth analysis of staff perspectives on working with underrepresented groups.
We learnt that the following were barriers to access:
- Lack of awareness of the service within the borough (residents and referrers)
- Barriers in communication between the service, referrers and service users (including language barriers, previous difficult experiences with NHS services)
- Practical barriers to access e.g. difficulties with accessing either online or in person appointments (e.g. due to work / caring commitments, mobility issues)
- Therapists do not represent the full range of residents in the borough – although the team is diverse in terms of ethnicity, there are not many male therapists, and there are some ethnicities not well represented in the team, e.g. Black British, African, Caribbean
- Feeling that some staff do not fully understand or proactively discuss issues of race, culture, religion with service users
- Feeling that some staff do not have a good enough understanding of how particular needs may impact service users, e.g. older adults, autistic people
- Feeling uncomfortable in mixed group settings
By integrating these insights, we aimed to develop a project that would address barriers to access and improve the experience of diverse client groups within the PTS. We believed that by enhancing their understanding of the unique needs and experiences of these underrepresented populations, we could develop targeted strategies to improve engagement and retention in therapy.
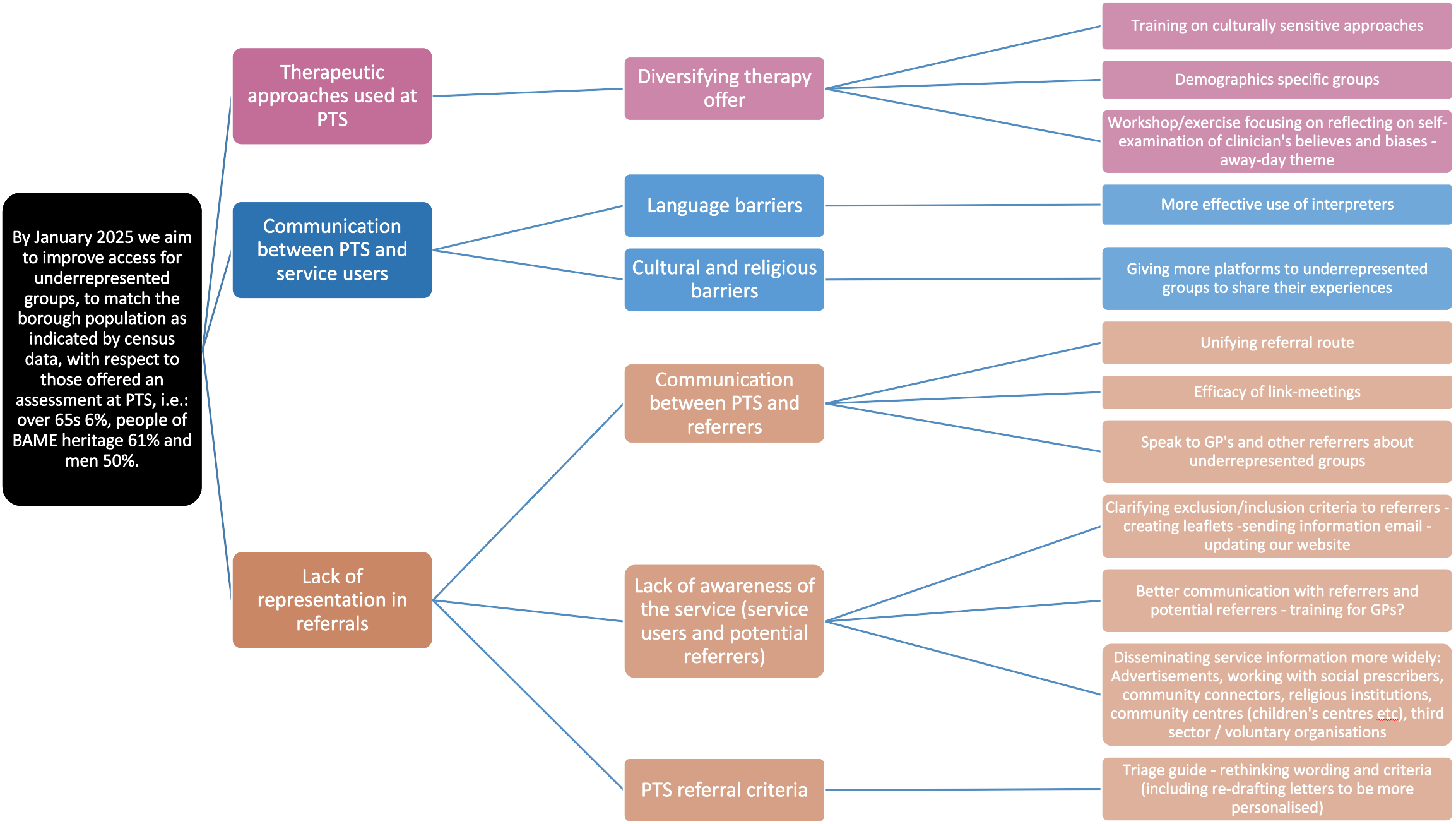
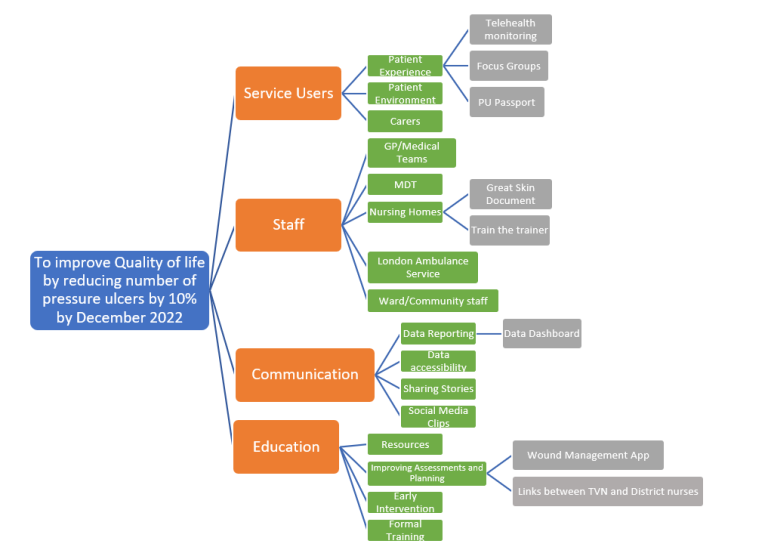
Once our team had spent time understanding the problem, we went on to develop our theory of change by using a tool called a driver diagram (See Figure 2)
Figure 2: Tower Hamlets PTS driver diagram
The team went on to test the following changes:
- Changes to the opt-in process: It was recognised that some groups of the community including older adults, people requiring an interpreter, and people with learning disabilities may require a different means of communication to enable them to access PTS. This change involved giving a phone call to these groups of people, if they did not respond to the initial opt-in contact sent to them via text message. This enabled staff members to talk these individuals through the service being offered and clarify any information which may not have been understood in the initial opt-in communication. This was tested for 3 months and led to an improvement in the percentage of older adult patients who opted in to the service, which was collected as a process measure.
- Incorporating training on biases into triage process: Staff training and away afternoons, including attendance of borough-wide Cultural Awareness Training were held to explore biases in clinical decision-making. The learning from this training has been incorporated into the team’s new triage pilot which they predict will support with increasing the proportion of people from underrepresented groups being offered an assessment. Ongoing monthly anti-racist practice meetings are also taking place to ensure these conversations continue to be had within the team.
- Offering demographic specific groups: There is an ongoing review of therapy groups, including delivering a trauma group for people from racially minoritised backgrounds, and a trauma group for women. By introducing these additional groups, it is predicted that people from underrepresented groups would feel more comfortable accessing the service. DIALOG scores, qualitative feedback and group dropout rates were monitored to determine the impact of these groups. There was strong positive feedback from the female-only groups which indicated that having single sex groups were helpful. However, there was still a low number of men on waiting lists and their dropout rates were higher.
- Change in referral criteria: We have tested changes to our referral criteria including having a more flexible approach where substance use and housing issues are no longer exclusion criteria and cases are reviewed on a case-by-case basis. We have also redrafted letters to make them more personalised and easier to understand.
- Change to triage process: Alongside the change in referral criteria, we also tested a joint triage process in collaboration with Stepney and Wapping Neighbourhood Mental Health Team (NMHT) and Tower Hamlets Primary Care Network (PCN) 9, to improve collaborative decision making on referrals and build closer links between PTS, the NMHT and PCN. This test was carried out for 4 months and we saw early signs of an increase in the proportion of referrals for men that are accepted by the service. This new triaging process was well received by the team, and it was acknowledged that as the referral criteria becomes more flexible there are great benefits to having joint discussions between PTS, NMHT and PCN colleagues. This change has now been implemented within all NMHTs where referrals are triaged in small groups of PTS practitioners – each NMHT now has 1 group dedicated to it.
Learning and next steps:
In order determine whether the changes we have tested have led to an improvement, we have been monitoring the percentage of underrepresented groups being offered as outcome measures (See Figures 3 to 5).
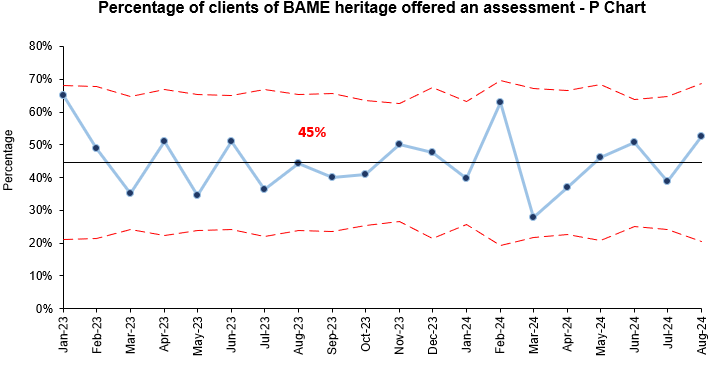
Figure 3: P Chart showing percentage of clients of BAME heritage offered an assessment
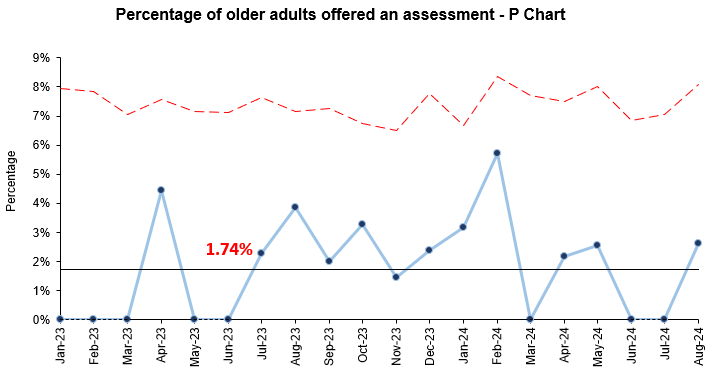
Figure 4: P Chart showing percentage of older adults offered an assessment
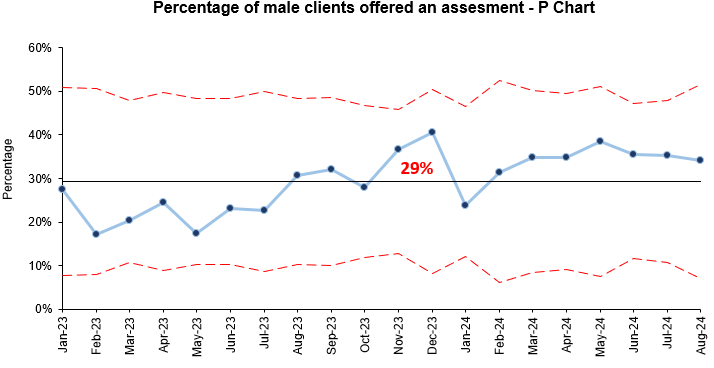
Figure 5: P Chart showing percentage of male clients offered an assessment
While we have not yet seen improvements in the outcome measures, we have seen some improvements in some of our process measures such as increase in the percentage of older adults who opt in. Additionally, we have received valuable insights into the barriers to accessing the PTS service and have received positive feedback on the changes that have been tested. To drive this work forward, we plan to:
- Revisit our driver diagram and data and consider creating smaller work streams which focuses on increasing access for individual underrepresented groups
- Track the types of referrals we are receiving from the NMHTs to gain an understanding of the demographics in their localities vs the referrals we are receiving. We have seen the benefits of joint triaging with NMHTs and PCNs and this data will be helpful in understanding which NMHTs we may need to work more closely with to increase the referrals we are receiving for underrepresented groups.
- Continue to build closer links with local organisations and services to gain further understanding of barriers for referrers and service users in accessing PTS and explore opportunities for more targeted approaches to increase referrals for under-represented groups.
- Continue co-production work with PTS service users to review what the service offers and how we can continue to improve communication between PTS and service users from different demographics.
- Continue to review referral criteria to reduce barriers to access and improve equity.
Most Read Stories
-
Why is Quality Control important?
18th July 2018

-
2016 QI Conference Poster Presentations
22nd March 2016
-
Recognising Racism: Using QI to Help Take Action
21st January 2021

-
QI Essentials: What does a Chief Quality Officer do?
18th March 2019

-
Using data enabled us to understand our problem
31st March 2023

-
The Power of Data in Reducing Pressure Ulcers
12th January 2022

Follow QI on social media
To keep up to date on the latest concerning QI at ELFT, follow us on our socials.