Steps Toward Better Access to Foot Health in Newham
9th July 2025
Written by Matthew Hosford (Senior Administrator), Marie Parchment (Clinical Lead Podiatrist) and Clarissa Sørlie (Improvement Advisor)
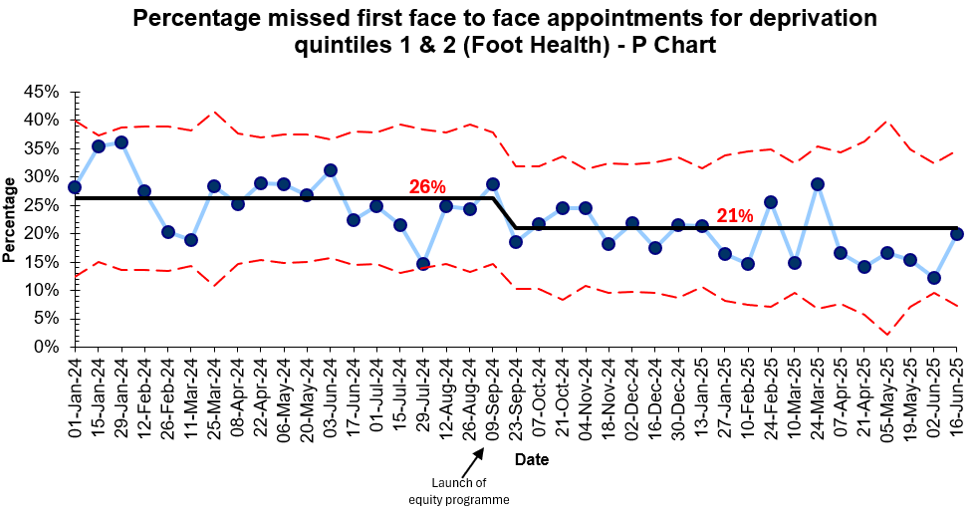
The Foot Health team in Newham have successfully achieved their aim of offering 90% of patients a first appointment within 18 weeks. This is very close to the 92% standard highlighted in the government’s new 10-year health plan (HM Government, 2025) and is higher than the London average of 61% (NHS England, 2025). They have also reduced missed first appointments by a fifth, enabling them to see patients quicker and make the best use of their resources.

Figure 1. Newham Foot Health team
The cancellation of face-to-face appointments during the Covid-19 pandemic, coupled with a national shortage of podiatrists (Royal College of Podiatry, 2021), led to a backlog of almost 2,000 patients waiting to be seen by the Newham Foot Health service in 2022/3. These patients presented with a range of conditions including diabetic foot ulcers, corns and calluses, musculoskeletal problems and ingrowing toenails. The team worked tirelessly to reduce the waiting list; however, by September 2024, just over half of patients (55%) were seen within the government target of 18 weeks.
Long waits for treatment can have serious consequences for patients. They may experience increased pain and discomfort, a decline in their overall wellbeing, and in some cases, a worsening of their condition. Timely access to care is especially critical for high-risk patients, as delays can lead to deterioration or complications. For example, people with diabetes are at greater risk of developing painful ulcers or requiring amputations if they are not seen quickly. Meeting the 18-week referral-to-treatment target ensures that patients receive the care they need when they need when they need it, reducing the risk of harm and easing the anxiety caused by prolonged uncertainty.
Patients from marginalised communities often face additional disadvantages when waiting times are long. Prolonged delays in treatment can affect their ability to work – particularly in jobs that require extended periods of standing or walking – impacting both their income and quality of life. They may also incur additional costs, such as paying for transport to avoid the pain or discomfort from walking. Furthermore, access to private podiatry services may be limited for those who can’t afford to pay for care, leaving them with fewer options and potentially worsening health outcomes.
These patients are also more likely to miss scheduled appointments, often due to circumstances beyond their control. Travel costs can be a significant barrier, particularly for those on low incomes. Older adults who rely on the Freedom Pass travel scheme may be unable to attend appointments scheduled before their pass is valid. Those in unstable or precarious employment may struggle to take time off work without risking their income or job security. Additionally, language barriers can prevent some patients from fully understanding the purpose of their appointment or from knowing that advocacy or interpretation support is available.
Recognising that over a quarter of their first appointments were lost due to non-attendance, the team formed a quality improvement (QI) project and joined the ELFT large-scale equity programme to reduce missed appointments. You can read about the early steps of their journey here.
Over 90% of patients are now seen within 18 weeks before their problems worsen (see Figure 2) and missed first appointments have fallen by 20% (see Figure 3). The team attribute this success to booking appointments over the telephone and verbally agreeing a date that suits the patient, proving that sometimes the simplest ideas are the most effective.
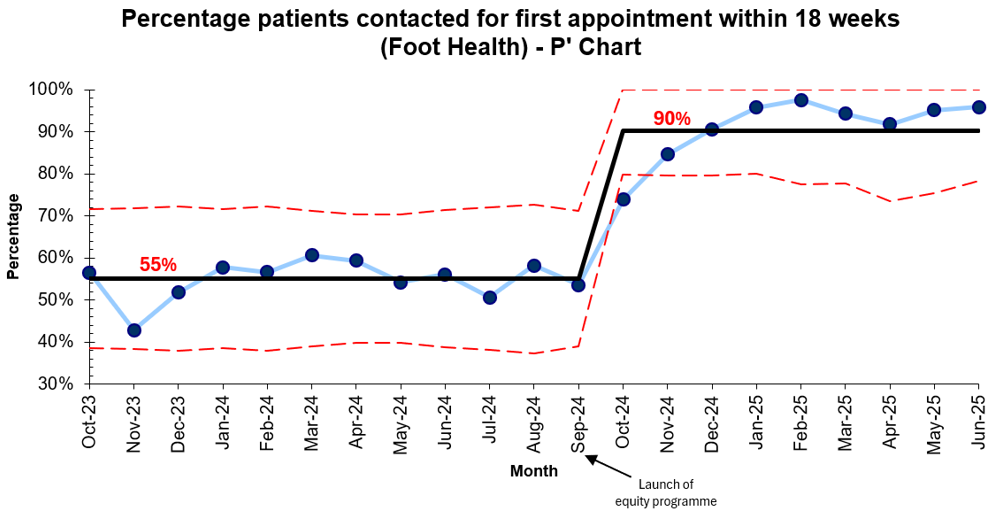 Figure 2. Control chart showing a 64% increase in patients contacted for a first appointment within 18 weeks
Figure 2. Control chart showing a 64% increase in patients contacted for a first appointment within 18 weeks
Figure 3. Control chart showing an 20% decrease in missed first appointments in Newham’s most deprived neighbourhoods
Reflecting on this QI project, Senior Administrator Matthew Hosford said, “Reaching these targets has had a huge impact on the team. Not only has it been morale-boosting for everyone to see such great results from their hard work, but it has also been rewarding knowing that people are getting the treatment they require at in reasonable timeframe.”
“The hard work, resilience and commitment of our admin staff has made this possible, and I would like to give a massive shout out to Amanda Demmer, Amanda Marsh and Noshin Amin for everything they have done over the last year with the foot clinic. Lastly, I must acknowledge the Podiatrists. If it wasn’t for their amazing work treating patients, all of this wouldn’t have been possible.”
The Foot Health team is committed to reducing missed appointments even further and has set an ambitious target to reduce them to just 8%.
References:
HM Government (2025) Fit for the Future: 10 Year Health Plan for England [online]. Available at: https://assets.publishing.service.gov.uk/media/6866387fe6557c544c74db7a/fit-for-the-future-10-year-health-plan-for-england.pdf (Accessed: 8th July 2025)
NHS England (2025) NHS in London continues to reduce waiting lists [online]. Available at: https://www.england.nhs.uk/london/2025/05/22/nhs-in-london-continues-to-reduce-waiting-lists/ (Accessed: 30th June 2025)
Royal College of Podiatry (2021) Saks Report: The Report of the Royal College of Podiatry Workforce, Education and Development Strategy Group [online]. Available at: https://heyzine.com/flip-book/saksreport.html (Accessed: 30th June 2025)
Most Read Stories
-
Why is Quality Control important?
18th July 2018

-
An Illustrated Guide to Quality Improvement
20th May 2019

-
2016 QI Conference Poster Presentations
22nd March 2016
-
Recognising Racism: Using QI to Help Take Action
21st January 2021

-
Using data enabled us to understand our problem
31st March 2023

-
QI Essentials: What does a Chief Quality Officer do?
18th March 2019


Follow QI on social media
To keep up to date on the latest concerning QI at ELFT, follow us on our socials.