“We Had to Think Outside the Box”: Improving Adherence to Continence Treatment Plans Among Bengali Women
31st July 2025
Written by Chinny Ejiogu (Continence Lead for Tower Hamlets Community Health Services), Nike Bademosi (Head of Clinical Services in Tower Hamlets) and Clarissa Sørlie (Improvement Advisor)
Pelvic health can have a profound impact on a person’s dignity, daily functioning, and independence. Yet for many Bengali women, cultural stigma, language barriers, and service design that doesn’t reflect their lives have meant limited engagement with continence services. The Tower Hamlets Continence team (see Figure 1) recognised that a different approach was needed to support Bengali women to adhere to their pelvic health treatment plans and see meaningful improvement. They set up a quality improvement (QI) project, with the aim of increasing the percentage of Bengali women who are adhering to their treatment plan from 45% to 60% by July 2025.
Figure 1. Continence team. From left to right: Nkechi Ochulo, Chinny Ejiogu and Funmilayo Oyelayo
Understanding the Problem
The issue was clear: women were staying on the continence service caseload for years – sometimes five or six – without any improvement. The common thread? They weren’t following through with their treatment plans and completing their pelvic floor exercises.
Rather than place blame, the team sought to understand why. Through listening to patients and completing a cause-and-effect diagram, they uncovered key barriers:
- Language: Many patients didn’t speak English fluently and were unable to understand the leaflets or instructions provided. Relying on family to translate was often not an option due to embarrassment or stigma.
- Appointment timing: Morning appointments often clashed with the school run, or were too early for patients taking sedating medications.
- Awareness: Both patients and referrers lacked clear information about the continence service, what it offered, and how it could help.
Nike Bademosi (Head of Clinical Services in Tower Hamlets) reflected, “If patients are not properly engaging with their care plan, they wouldn’t see an improvement, and our caseload would just continue to increase. We need to think outside the box.”
Why Pelvic Health Matters
Pelvic health is often under-discussed and under-prioritised, but its impact is wide-reaching – for example, influencing self-esteem, affecting participation in social activities and straining relationships (Bladder and Bowel UK, 2024). A study by the Royal College of Obstetricians and Gynaecologists (2023) revealed that one in five of people surveyed experienced urinary incontinence, yet over half did not do pelvic floor exercises which could improve or prevent symptoms. For Bengali women, embarrassment and cultural stigma can lead to years of suffering in silence, not knowing that help is available (Mallick et al. 2023). Education, access, and trust-building are therefore crucial.
What We Changed
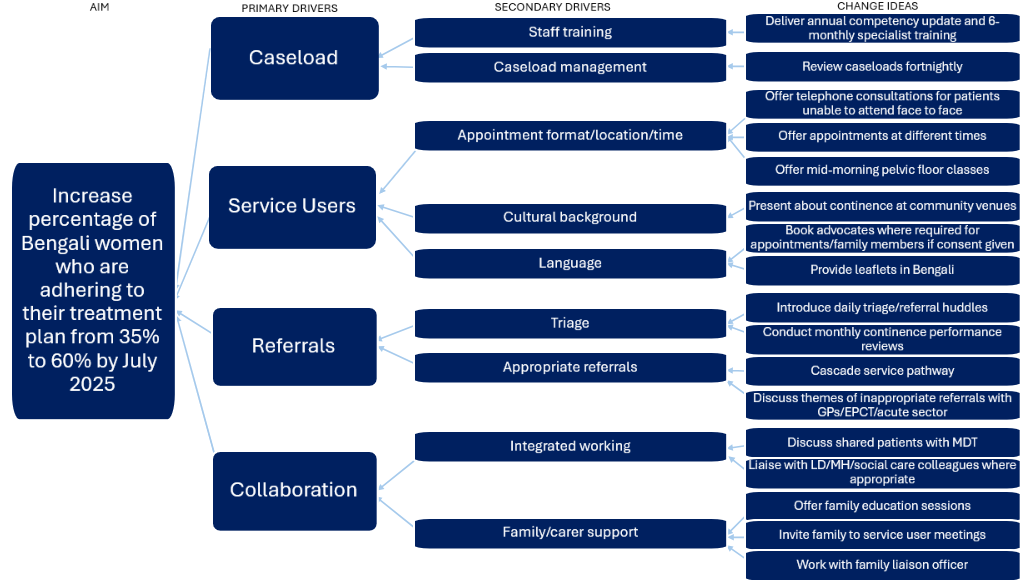
Using quality improvement methods, the team tested and refined a range of change ideas (see Figure 2) aimed at removing barriers and building trust:
- Introduced Bengali-language continence classes with a Bengali-speaking advocate to improve understanding and comfort.
- Changed the class time to 10am, making it easier for parents and those on sedating medications to attend.
- Created leaflets in Bengali, allowing women to learn about pelvic floor exercises and stress incontinence privately, without relying on family members.
- Held focus groups and community outreach at Bengali women’s groups to raise awareness and answer questions.
- Strengthened relationships with local GPs, educating them on the benefits of early referral and adding clear guidance to the service’s website.
- Enabled patients to track progress, using clinical assessments at their first and third appointments to demonstrate improvement.
- Introduced a new device (Diveen) – a drug-free pelvic floor support product available on prescription – which many women found easy to use and side-effect free.
- Encouraged treatment adherence during Ramadan, helping patients stay on track even while fasting.
- Expanded class capacity from 10 to 15 places due to increased demand.
Crucially, a Bengali woman with lived experience of the service joined the improvement team, providing insight into why appointments were missed and ensuring changes were culturally relevant and likely to succeed.
Figure 2. Driver diagram outlining the team’s theory of change
What We Learned
This project offered powerful lessons about delivering culturally responsive care:
- Understand the barriers, then design your changes around them.
Recognising that there might be a reason for non-compliance with a treatment plan. - Build trust, not just treatment plans.
Spending a few extra minutes listening, validating, and co-planning with patients helped break down resistance and encouraged long-term engagement. - Get out of the clinic.
Outreach was essential – people will not benefit from a service they are not aware off. Visiting community spaces helped the team educate, listen, and learn from the outreach. - Involve people with lived experience.
A service user on the project team shaped the project’s direction and helped ensure changes truly worked for patients. - Empower patients to self-manage.
By the end of treatment, patients were confident to continue their exercises at home, reducing the need for long-term support.
Through their hard work and culturally sensitive approach, the team achieved a significant improvement in treatment adherence – increasing it from just 35% at baseline to 90% by the end of the project (see Figure 3). This exceeded their original aim of 60% and demonstrated that by removing barriers, building trust, and engaging meaningfully with the community, it is possible to support patients to take ownership of their pelvic health and successfully follow through with their treatment plans.
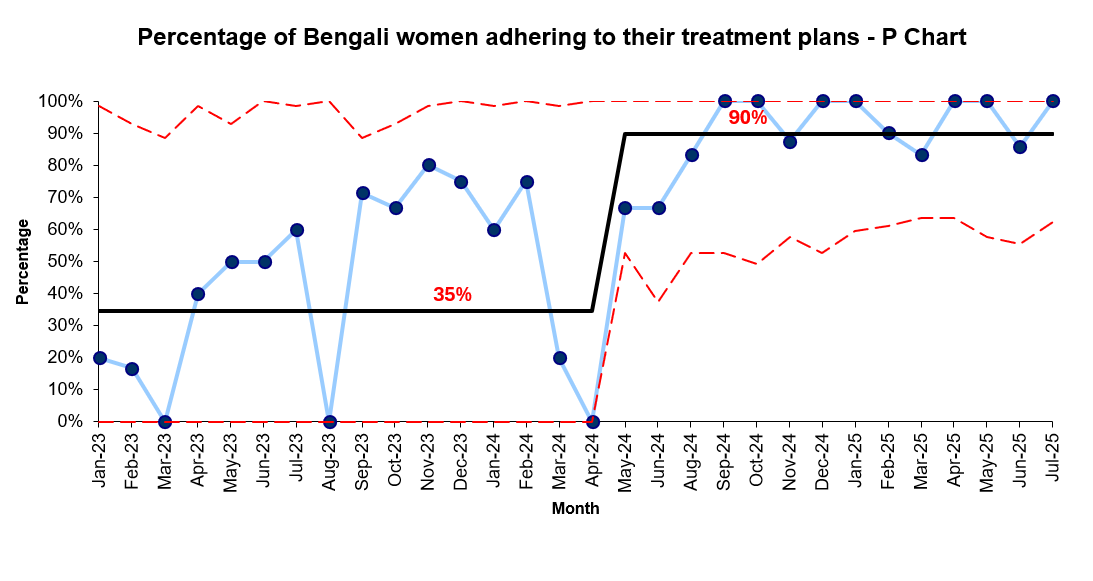
Figure 3. Control chart showing an increase in treatment adherence from 35% to 90%
Continence Lead Chinny Ejiogu shared: “I couldn’t have done this without my wonderful staff – we elevated pelvic floor care to a whole new level.”
What’s Next
Although the improvement project has officially concluded, the team continues to monitor data through clinical meetings and review individual cases to ensure ongoing support. The next phase includes outreach to acute services, gynaecology clinics, and antenatal departments, starting with providing Bengali-language leaflets for waiting areas and exploring future partnerships.
By rethinking how continence care is delivered and removing barriers rooted in language, stigma, and service design, this project has not only helped women improve their pelvic health – but it’s also built a bridge between clinical care and community connection.
To learn more about the Tower Hamlets continence service, listen to this podcast episode
References:
- Bladder and Bowel UK (2024) ‘Supporting someone with incontinence: Shining a light on the impact on families’ [Online]. Available at: https://www.bbuk.org.uk/supporting-someone-with-incontinence-shining-a-light-on-the-impact-on-families/ (Accessed: 28th July 2025)
- Mallick, S., Akterm S., Islam, S. and Biswas, PK (2023) ‘Urinary Incontinence in Bangladeshi Women: A Cross-Sectional Analysis of Prevalence, Cultural Perceptions, and Quality of Life Implications’, Asian Journal of Research and Reports in Urology, 6(1), pp. 136-140. Available at: https://journalajrru.com/index.php/AJRRU/article/view/106/209 (Accessed: 28th July 2025)
- Royal College of Obstetricians and Gynaecologists (2023) ‘RCOG calling for action to reduce number of women living with poor pelvic floor health’ [Online]. Available at: https://www.rcog.org.uk/news/rcog-calling-for-action-to-reduce-number-of-women-living-with-poor-pelvic-floor-health/ (Accessed: 28th July 2025)
Most Read Stories
-
Why is Quality Control important?
18th July 2018

-
An Illustrated Guide to Quality Improvement
20th May 2019

-
2016 QI Conference Poster Presentations
22nd March 2016
-
Recognising Racism: Using QI to Help Take Action
21st January 2021

-
Using data enabled us to understand our problem
31st March 2023

-
QI Essentials: What does a Chief Quality Officer do?
18th March 2019


Follow QI on social media
To keep up to date on the latest concerning QI at ELFT, follow us on our socials.