
From Observation to Engagement: replacing routine checks with meaningful connections
14th May 2025
Senior leaders from across East London NHS Foundation Trust came together in May for a focused workshop on the Trust’s new programme to eliminate intermittent observations on our inpatient wards. The session introduced the programme’s emerging theory of change, sought expert feedback on its execution theory, and explored the cultural shift required to move from observation to embedding more therapeutic forms of engagement. We were delighted to welcome Professor Jason Leitch from the Institute for Healthcare Improvement who shared valuable reflections on programme design, supporting staff through change, and the importance of proactively managing risks along the way.
Why this work matters
Intermittent observations have been a long-standing feature of mental health care, typically used to monitor individuals perceived to be at risk. However, growing evidence and feedback from both staff and service users suggest that this practice often brings unintended harms. These can include disrupted sleep, loss of privacy, and missed opportunities for therapeutic connection.
Building on previous efforts to standardise observation practices, this new programme aims to go further: to eliminate the use of intermittent observations, while strengthening safer, more compassionate forms of care. Instead of relying on scheduled checks, the focus will be on creating ward environments where relational, therapeutic engagement is the default.
There’s also a strong financial case. In 2023/24, ELFT spent £16.58 million on bank staffing for acuity and enhanced care, with £5.5 million attributed specifically to observations. Intermittent observations are often used in response to perceived risk but may not contribute meaningfully to outcomes. By reducing reliance on this practice, the programme aims to unlock projected savings of £3.77 million in the coming financial year—funds that could be better invested in sustainable, high-quality care.
The programme design
As part of the session, we explored the programme’s initial theory of change—developed through a review of the evidence on therapeutic engagement and observations, alongside early conversations with inpatient teams. This theory will continue to evolve as we learn more. In particular, we’ll be using local data to identify whether specific groups of service users may need tailored support as we move away from intermittent observations, ensuring the approach is equitable, safe and responsive to individual needs.
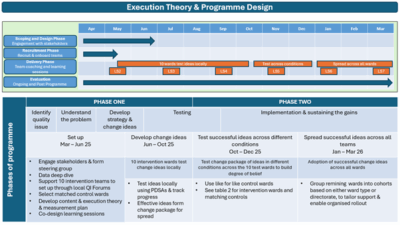
The programme will be delivered in two phases, aligned with the IHI framework for going to full scale:
- Phase 1 (April – October 2025): Ten inpatient wards will test new approaches to reducing intermitten observations with hands-on support from local Improvement Advisors, QI coaches, and sponsors. A live Power BI dashboard will provide real-time data to guide decision-making and monitor impact.
- Phase 2 (November 2025 onwards): The most effective ideas will be refined and tested in new conditions to build confidence in their effectiveness. Once a strong degree of belief is established, these changes will be spread across all ELFT inpatient wards using a structured approach to scale.
Test wards will be paired with control wards to help understand the true impact of changes. Teams will meet regularly to learn from each other, share successes, and overcome challenges together.
Key measures include:
- The number of service users on intermittent observations
- Rates of safety incidents (e.g. aggression, seclusion, restraint, self-harm)
- Bank staffing levels
- Service user experience of care
Learning from the event
The session sparked rich discussions about the culture change needed to shift from observation to engagement. Several key themes emerged:
- Language matters. Framing this work around “therapeutic engagement” helps shift the focus from risk management to relational care—and gives teams permission to do things differently.
- Support for staff is essential. Staff need time, space, and leadership backing to feel confident in moving away from long-standing practices. Face-to-face connection, encouragement, and shared learning will be vital.
- Co-design is non-negotiable. Bringing service users into the design process from the start will help ensure changes are meaningful, respectful, and grounded in lived experience.
What’s next?
This session marked an important step in what will be a Trust-wide journey over the next year. While the work will be challenging, there is a shared commitment to redesigning care in ways that feel safer, more relational, and more purposeful for everyone involved.
Next steps include bringing together the ten participating teams for their second shared learning session, where they’ll analyse their local data, explore the drivers behind current practice, and begin testing high-impact ideas to reduce reliance on intermittent observations.
Most Read Stories
-
Why is Quality Control important?
18th July 2018

-
An Illustrated Guide to Quality Improvement
20th May 2019

-
2016 QI Conference Poster Presentations
22nd March 2016
-
Recognising Racism: Using QI to Help Take Action
21st January 2021

-
Using data enabled us to understand our problem
31st March 2023

-
QI Essentials: What does a Chief Quality Officer do?
18th March 2019


Follow QI on social media
To keep up to date on the latest concerning QI at ELFT, follow us on our socials.



