
How East London NHS Trust Improved Flow and Achieved £8.6 million in Projected Cost Avoidance
21st January 2025
By Sarah McAllister (Head of Improvement Programmes)
At East London NHS Foundation Trust (ELFT), our focus has always been on improving the quality of life for those we serve, but what if better care could also mean better use of NHS resources? In April 2024, we set out to improve patient flow with two key aims: eliminate out-of-area placements and reduce length of stay to 40 days—keeping people closer to home while managing hospital care more effectively.
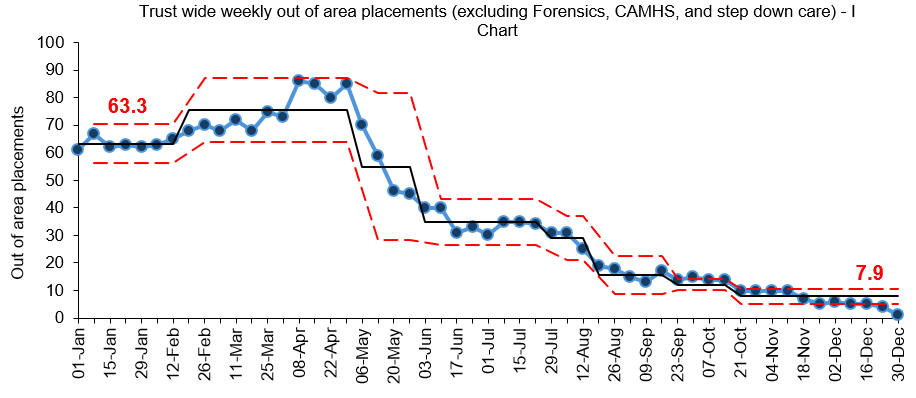
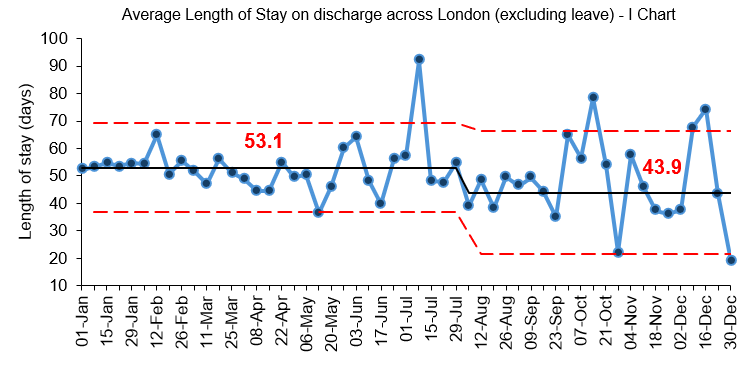
Just months later, teams have achieved substantial improvements: trust wide out of area placements have all but been eliminated to one a week, length of stay across London has been reduced by 17% and £8.6 million in projected costs have been avoided this year.
How did we get here? Let’s take you on the journey…
The Patient Flow Pathway: Small Changes, Big Impact
The programme didn’t rely on one big idea, but a series of practical changes tested across the patient pathway. Supported by data-driven decisions, these changes ensure service users receive the right care, at the right time, in the right place.
1. Pre-admission / referral
The focus here is on creating options that help people avoid unnecessary hospital admissions. Services like step-up beds in Newham or a crisis house in Tower Hamlets offer alternative care options early on.
2.Triage
At triage, teams identify the best care pathway for each patient. Initiatives like a dedicated triage ward in Newham and the Home Treatment Team in City & Hackney ensure timely decisions and help prevent avoidable admissions, both within ELFT and out of area.
3. Admission
Daily routines such as red-to-green huddles and bed escalation meetings, ensure timely decisions on patient care and discharges can be made. Alongside these daily huddles, weekly meetings with senior leaders including clinical and borough directors, borough lead nurses, matrons, ward managers, social workers, consultants and community team managers enable more joined up decision making and senior support to resolve barriers to discharge.
4. Discharge
At discharge, services like step-down beds in Bedford and Luton, and discharge-to-assess beds in Tower Hamlets allow service users deemed clinically ready for discharge to continue recovery in appropriate settings while addressing social care or housing needs.
Several key principles supported the practical delivery of these ideas.
- Culture shift
- Clear direction from senior leaders reinforces the purpose of admission, step-up, and step-down beds.
- Collaboration is key
- Working closely with system partners—social care, housing, local authorities, and supported accommodation—to streamline patient journeys.
- Daily discussions
- Real-time problem solving through daily conversations keeps flow on track.
- Adjusting to demand
- Flexibility was crucial with daily flow discussions at the peak of the crisis.
- Data driven decision making
- Regularly reviewing data helps teams monitor progress, identify delays, and act quickly.
From Big Challenges to Big Savings
Out of area placements are both tough on service users and their families, and costly to services. Before the programme began, the Trust faced high monthly spend on these placements. Trust wide we’ve dramatically reduced spend on out of area private beds by 93%, from an estimated average of £370,937 per week to £24,572 per week, with this being at a low of £4,563 in the last week of December 2024.
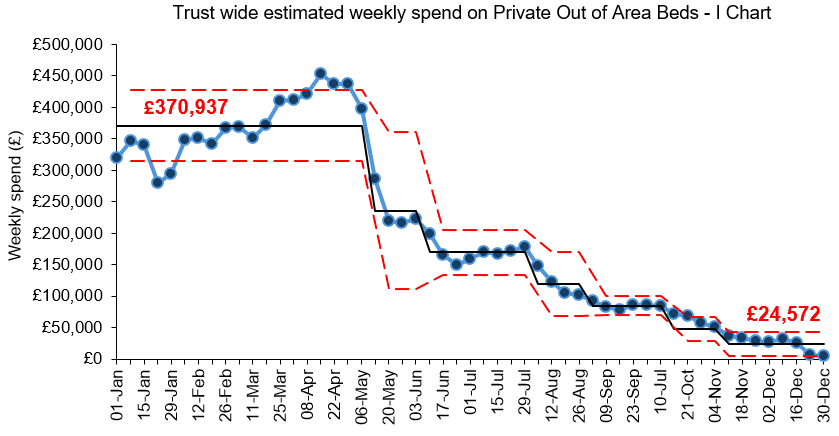
To keep ourselves on track, we developed an agreed financial framework to quantify the impact of this work. Comparing our current monthly spend (run rate) against a baseline from earlier this year (April 2024 to July 2024), we are projecting £8.6 million in cost avoidance across the Trust for the year. In some areas of the trust, we are now offering inpatient mental health bed capacity to other organisations.
This isn’t just a number—it’s a reflection of improved patient experiences, efficient care, and a system working smarter to deliver better outcomes.
What This Means for the Future
By working to all but eliminate out of area placements, streamlining care pathways and tackle Length of Stay, ELFT has not only saved costs but set a blueprint for better patient care. This is a journey of innovation, collaboration, with results including:
- Substantial trust wide reduction in out of area bed use from a high of 86 each week to 1 a week.
- £8.6 million in projected cost avoidance
- 93% reduction in trust wide spend on out of area placements.
- 17% reduction in length of stay across East London to an average of 41 days.
- 44% reduction in trust wide instances of clinically ready for discharge.
- Reduction in trust wide bed occupancy from 105.5% to 94%.
What’s next? We are currently in the process of developing a change package of ideas and updating our local inpatient policies to reflect our new ways of working.
Most Read Stories
-
Why is Quality Control important?
18th July 2018

-
An Illustrated Guide to Quality Improvement
20th May 2019

-
2016 QI Conference Poster Presentations
22nd March 2016
-
Recognising Racism: Using QI to Help Take Action
21st January 2021

-
Using data enabled us to understand our problem
31st March 2023

-
QI Essentials: What does a Chief Quality Officer do?
18th March 2019


Follow QI on social media
To keep up to date on the latest concerning QI at ELFT, follow us on our socials.


