
Improving physical health for people taking antipsychotic medication
11th August 2015
 This month we caught up with Dr Helen Thomson from Specialist Services to find out about their QI project aimed at improving physical health for people taking antipsychotic medication in the Community Learning Disabilities Service.
This month we caught up with Dr Helen Thomson from Specialist Services to find out about their QI project aimed at improving physical health for people taking antipsychotic medication in the Community Learning Disabilities Service.
How did you identify the improvement idea for your project?
A previous trainee carried out an audit which demonstrated low compliance with the recommended monitoring of physical health side effects from antipsychotics according to NICE. We had also informally noticed that certain equipment was not available and systems were not in place to easily hand over the information about monitoring to incoming doctors and easily communicate it to GPs. We were also aware that there are a lot of community programs which aim to improve cardiovascular health through diet and exercise but we sometimes weren’t aware which programs are still running, which are suitable for people with learning disabilities and how we refer our patients. This might have impeded the discussions about diet and exercise if clinicians did not feel confident that there would be a suitable management option available.
Did you identify any barriers to your project? if so how did you overcome them?
We found that clinicians were carrying out monitoring in an ad-hoc manner, when they noticed something was overdue. This means that each patient might have had measures assessed at different times of year. This made it fairly slow to find the information which affecting the QI data collection but made it difficult for clinicians to notice when monitoring is overdue. We therefore changed the approach to monitoring to make it a structured, yearly screen which should be documented in a designated section of the clinic letter and this section is pre-populated so that is it more clearly obvious when the next check is due. This saved time with the data collection, which had been a significant barrier to the project.
Other barriers included around the finding out what issues affected patients getting blood tests. I tried to carry out process mapping of ten patients who didn’t have results available. I discovered that some of these patients had in fact had blood tests and the results were on a different pathology system. Therefore quite small numbers of patients actually hadn’t had a blood test so improvements in this area would result in quite a small change. Numbers remained low when I carried out process mapping for all patients without blood results. The most obvious reason some patients hadn’t had a test was due to them being scared and therefore not compliant. In a few patients, other staff had become involved in a plan to carry out some desensitisation work with the patient. In most of the other patients who hadn’t had a test, we had asked the GP to arrange a blood test but no request had been sent and it was difficult to find out why. Perhaps this indicated some issues around communication with GPs however the numbers for this were very low.
What are your early results and latest data showing us?
Our early results show initial improvements across all measures with a subsequent slight drop in the results in June. The reasons for this drop might include a number of patients having had an appointment earlier in the QI period and having had their monitoring at this stage and therefore the clinician not wishing to repeat the monitoring. Clinicians each taking leave in the summer meant fewer patients were seen in this period, affecting the results.
The results are higher for patients seen in clinic, probably because of the height, weight and blood pressure equipment being there. Because of this we are thinking of ways to improve the collection of results for these measures during domiciliary visits. This might include portable equipment or better communication with GPs who tend to have this information for our patients from their learning disability annual health checks.
How has the QI training influenced the way you run your project?
I used the information on the QI microsite and IHI website to learn about the methodology and also had some really valuable advice from our QI coach, Genevieve Holt. We realised that our first plan was in fact, more of an audit in that it mostly targeted clinician behaviour and therefore might have not resulted in sustainable changes. We then tried to look at the systems and think a bit more radically about how to introduce a ‘change’ rather than a ‘task’.
We had also planned to collect data every 2 months as the data collection was quite a slow process. We realised this would not adequately inform us which changes had been responsible for any improvement as several changes would have been tested together. It would have been too slow to carry out successive trials of change ideas. We changed the planned data from the percentage of patients who had the recommended monitoring over the last 12 months, to the percentage of patients seen by any clinician over a 2-week period who had the monitoring during this time. 2-week cycles meant small changes could be tested and adapted more effectively.
Finally, how would you sum up your personal learning experience of QI and its benefits?
I found that QI methodology allowed me to think more imaginatively about the systems and how I would ideally design them. In QI, if a change seems sensible then you test it out on a small scale. Thinking in this way will hopefully help me try out solutions to problems in the future without worrying too much about the possible consequences.
It has also helped me realise the value of maintaining good working relations with other agencies and disciplines. The fact that most team members were happy to participate in this project was really helpful to the project and a valuable lesson in leadership skills.
Most Read Stories
-
Why is Quality Control important?
18th July 2018

-
2016 QI Conference Poster Presentations
22nd March 2016
-
Recognising Racism: Using QI to Help Take Action
21st January 2021

-
QI Essentials: What does a Chief Quality Officer do?
18th March 2019

-
Using data enabled us to understand our problem
31st March 2023

-
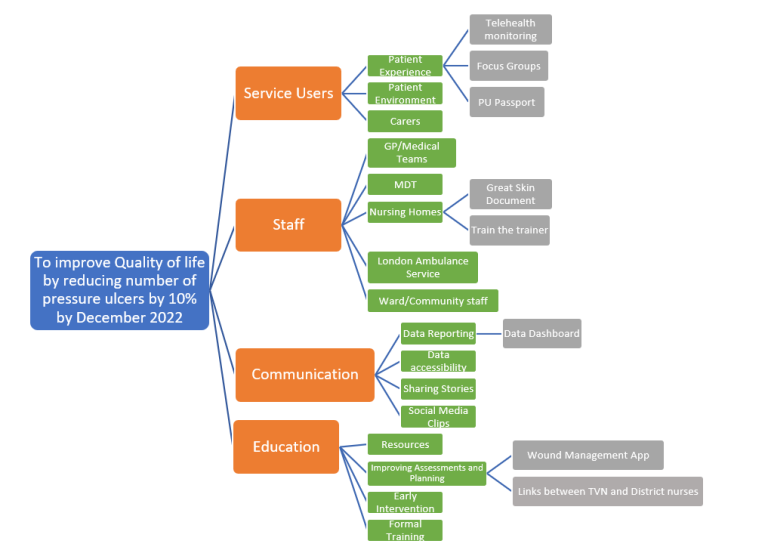
The Power of Data in Reducing Pressure Ulcers
12th January 2022

Follow QI on social media
To keep up to date on the latest concerning QI at ELFT, follow us on our socials.


