
Improving referrals of patients on clozapine to Luton Psychiatric Liaison Service (PLS)
20th January 2025
Written by Marisa Manning, Amit Pancha, Maria Filippidou, Mohammed Mumtaz, Barbara Tratsaert and Miles Tringham


What is Clozapine and why is it so important?
Clozapine is a medication used to treat the symptoms of psychosis. In the past, patients on clozapine have been admitted to hospital and the Psychiatric Liaison Service (PLS) have not been informed. This has resulted in patients not receiving their clozapine for 48 hours, therefore needing it to be re-titrated. If Clozapine is missed for 48 hours and then their usual dose is administered, serious side effects can occur.
Unnecessary re-titration has wide reaching impacts. Typically, it requires around a 17 day psychiatric admission. An estimated cost of this approximately £568.71 X 17 = £9668.07!
Beyond the cost pressure implications, this is also incredibly intrusive to the service user’s life; needing to have routine and environment completely changed, as well as experiencing clozapine symptoms all over again.
Mohammed, a lived experience expert and project team member, shares his experience of clozapine titration.
What’s it like to experience clozapine re-titration?
What many people don’t understand is that when you have to re-titrate clozapine, you experience all the symptoms all over again. It can take 4 weeks sometimes to return to feeling normal. I went through hell with it. During that time, I experienced really bad emotions. I was really tired, lethargic. It took a lot of perseverance for me to get through those 4 weeks. Having experienced the symptoms before, I knew it was possible to get through it, but it’s tough. I was fortunate enough to have support from my nurse who assured and encouraged me throughout the process. It made a massive difference. She was brilliant.
Re-titration requires a long stay on an inpatient ward, what was that like?
All you want to do is sleep at the time, because these motions are so bad. You’re separated from your home, family, friends, and yet all you want to do is sleep. Just sleep to get through it. It takes perseverance, but you get through it.
Something that’s often not considered is the amount of blood tests. When starting clozapine you’re getting constant blood tests. It’s quite intense. You must remember your body heals from it and it eventually becomes less frequent, down to every 2 or 3 days, then weekly, then monthly. When on clozapine you will always need to have monthly blood tests to check everything is all ok. Some people struggle with that though, they don’t like the constant tests, but it’s necessary.
Are there impacts of missing clozapine doses other than needing re-titration?
Insomnia. Straight away. Clozapine is such a good sleep aid; I feel it immediately if I miss a dose. I’m up all night which of course makes things worse. You don’t realise how well you can get a decent sleep routine with it. This is why most people take their dose in the evening, and then a little bit in the morning. That’s how they titrate on the ward too, for that reason. I suffer from restless legs, so without this medication I can be up all night and become more unwell because of it.
Another thing that isn’t talked about is the impact on bodily functions. It massively alters your digestive tract. Missing just one dose can cause some people constipation issues for up to 4 days. It’s horrible. It impacts everything. The other effect it has is on how you salivate. It greatly increases it, especially at night when you’re trying to sleep. It’s the little things, like at times, having to change pillowcases every single day. I think it’s important we talk about these things because it affects everyday life, and people would be in a better place if we were better educated and more open about it.
What are the benefits of using Clozapine?
Clozapine is has a lot of side effects and is really challenging, but I’m grateful for it. It’s worked for me where other medication hasn’t been effective. I can sleep. It helps me stay well. I was a calmer, nicer person because of it.
The Team
A team came together to tackle this issue as a QI project. The team is made up of a pharmacist, three psychiatrists in PLS, a service user with lived experience of clozapine and hospital use and a QI coach.
The situation
Over a 9-month period (October 2022 to June 2023), a total of 25 patients were prescribed clozapine using the Nervecentre electronic prescribing system, averaging 2.8 patients per month. Of these, 13 patients (52%) were referred to the PLS, with 10 (40%) being referred within 48 hours of hospital admission. However, 1 patient (4%) did not receive clozapine on Nervecentre within 48 hours and was also not referred to the Luton PLS.
The team set out with the aim “For 100% of patients on clozapine to be referred to PLS, within 48 hrs of their admission to hospital, by August 2024.” Then, broke down the problem into a driver diagram.
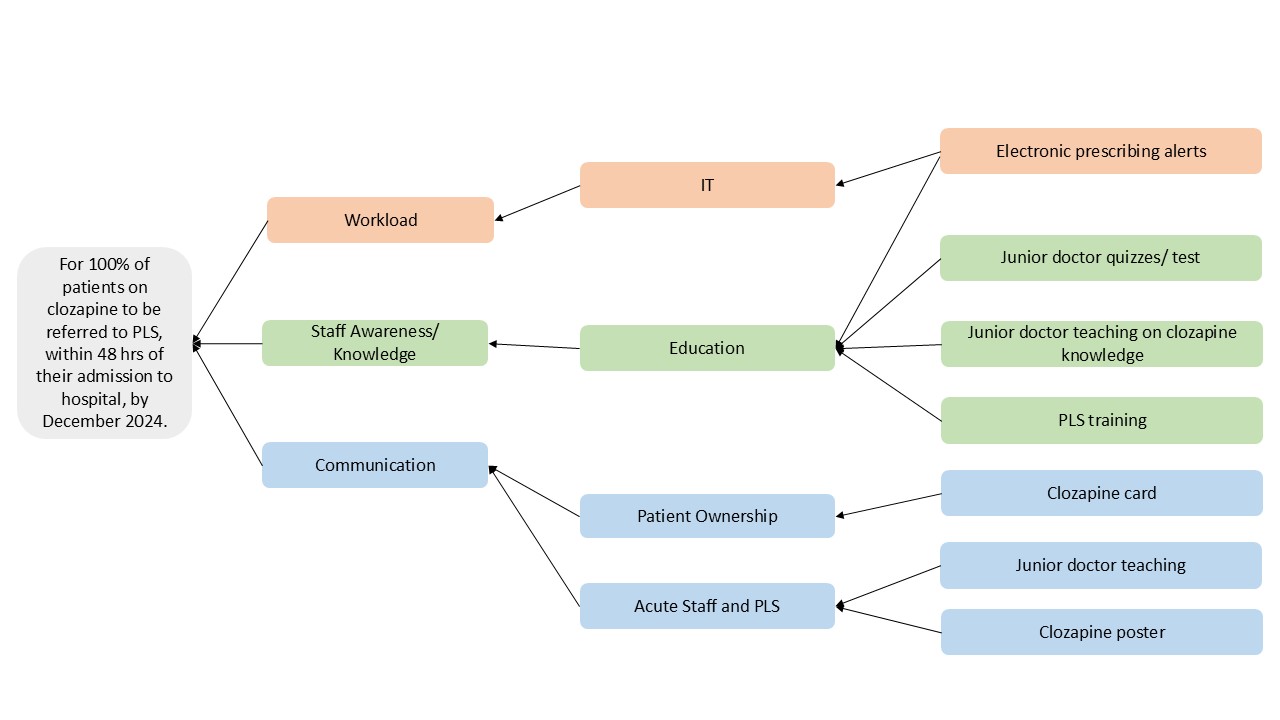
“Five key interventions were prioritised to improve referral rates, from the Emergency Department to ward admission. These included adding alerts to the electronic prescribing system, providing training for junior doctors and PLS staff, introducing the clozapine alert card, and developing educational posters for both staff and patients. The team met regularly to monitor progress, implementing system changes, educational materials, and guidelines. Additionally, a “clozapine management” option was incorporated into the RiO electronic patient health record system, and two educational posters were created to reinforce the new protocols.” – Marisa Manning, Consultant Psychiatrist in the Psychiatric Liaison Service, and joint project lead.
PDSAs – To Action!
The team ran a series of 4 PDSA (Plan, Do, Study, Act) cycles, focusing on Technology/ processes, Patient Experience, Education, and Communication.
Change Test 1
The first change idea tested introduced prompts into the hospital’s electronic prescribing system. This idea was suggested by junior doctors in hospital. These prompts reminded prescribers to refer all patients on to the Psychiatric Liaison Service (PLS). It then alerted staff to verify whether patients had received their last dose within 48 hours to prevent inappropriate administration.
Following this, a referral algorithm was created for PLS staff to ensure all referrals were accepted. This intervention resulted in a referral rate consistently above 75%, and the system prompts remain in place as business as usual.
Change Test 2
Following success in adapting the electronic prescribing systems, the team set out to address clinical knowledge and education. To improve clinician knowledge, educational materials were developed for both hospital and PLS clinicians, addressing gaps in understanding clozapine support. This included slides, a survey, and a guidance document. The intervention led to 100% referral rates in four of the next seven months. To sustain success, the educational sessions need to be repeated for each new cohort of Foundation Year doctors and PLS staff.
Change Test 3
This cycle focused on increasing patient awareness about the need for PLS referral upon hospital admission. A poster outlining clozapine side effects and hospital admission implications was displayed in clozapine clinics and shared with clinical staff. However, the impact of this intervention was limited, as it relied on the continued visibility of posters and clinician engagement, leading to minimal long-term effect.
Change Test 4
Although referral rates improved, timely referrals within 48 hours remained inconsistent. A focus group of Foundation Year doctors suggested adding an alert to the hospital’s electronic clinical notes as a solution. Additionally, a clozapine alert card, based on patient feedback, was proposed to help patients communicate their medication needs, though this change has not yet been tested.
Results and Into 2025
“When comparing baseline data to post-intervention results, the referral rate improved by 24%, increasing from 52% to 76%. Similarly, the rate of referrals made within 48 hours of admission increased by 12%, from 40% to 52%.” – Marisa Manning, Consultant Psychiatrist in the Psychiatric Liaison Service, and joint project lead.
Whilst there has been clear improvement, a sustained 100% referral rate is yet to be hit long-term; work continues! The team recognises the need for displaying data over time to understand the sustainability of improvements and variation within the system. The next step will be to work with hospital and pharmacy systems to review and organise data.
The number of referrals may be small, but thanks to the contributions of people like Mohammed we understand each case has massive potential consequences in health, wellbeing, and financial viability.
The team hopes to share their learning with other teams to support hospitals improve with them.
Maybe the next story will be one of “scaling up improvement”? Watch this space.
Most Read Stories
-
Why is Quality Control important?
18th July 2018

-
2016 QI Conference Poster Presentations
22nd March 2016
-
Recognising Racism: Using QI to Help Take Action
21st January 2021

-
QI Essentials: What does a Chief Quality Officer do?
18th March 2019

-
Using data enabled us to understand our problem
31st March 2023

-
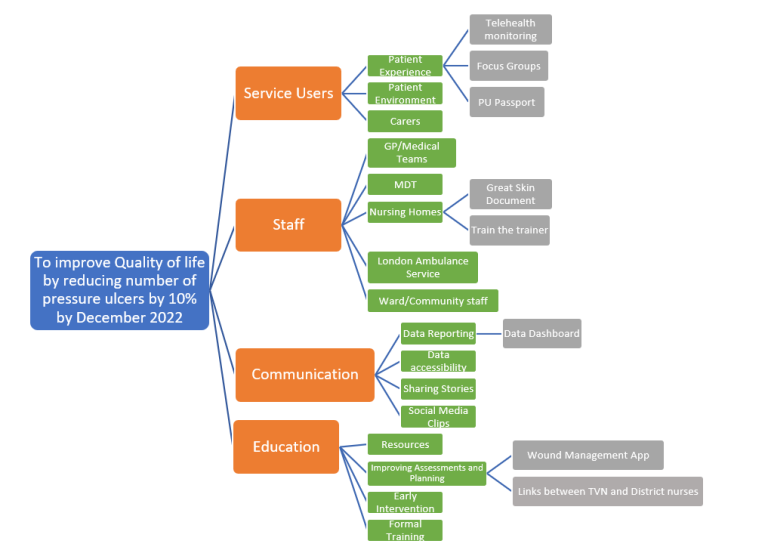
The Power of Data in Reducing Pressure Ulcers
12th January 2022

Follow QI on social media
To keep up to date on the latest concerning QI at ELFT, follow us on our socials.


