Making mealtimes safe and comfortable for all: spotting signs of difficulties swallowing in forensic inpatient services
10th March 2025
By Jena Hall, Speech and Language Therapist & QI Project Lead and William Diaz, Improvement Advisor
Did you know people with schizophrenia are more likely to die from choking than the general population? Or that medication side effects such as dry mouth & movement disorder can seriously impair swallowing?
ELFT forensic inpatient services at the John Howard Centre and Wolfson House provide care to almost 200 patients with support needs due to mental health (MH), learning disability and autism (LDA).
Speech and language therapy (SALT) has been a core part of the LDA wards multi-disciplinary teams for a number of years, but is a more recent addition to the MH wards provision. The forensics directorate’s increased investment in SALT was aimed to develop a dysphagia service to improve patient safety and improve population health.
What is dysphagia? Dysphagia is the medical term for discomfort or difficulties swallowing, which is more common for people with mental health needs or learning disability. Dysphagia can be serious patient safety issue with risks including respiratory infections, choking and death (RCSLT, 2023).
Introducing a small, new service within an established service model can be challenging. However, it also provided opportunity to develop the service flexibly and responsively. Referrals were initially sporadic, and often in relation to urgent or emergent care issues i.e. serious choking incidents or physical health hospital admissions. We decided to use quality improvement to explore this challenge.
We established a project team with several members attending ELFT Improvement Leaders Programme training together. Team members included Sean Denny (speech and language therapist), Iduna Heinrich (dietician), Curtis Reece (physical health nurse lead), and JG (service user). Team was supported by the Forensics SALT colleagues, Kutub Uddin (informatics), Chouna Smith (physical health nurse lead & project coach), Lawford Clough (project sponsor) and William Diaz (improvement advisor).
We wanted to capture the views and priorities from all key players – nurses, SALT service users and the multidisciplinary team (MDT). Using QI methodology, we spent time understanding dysphagia in mental health services and how to improve access to SALT support. The team met weekly, working with the MDT and a service user as a core team member.
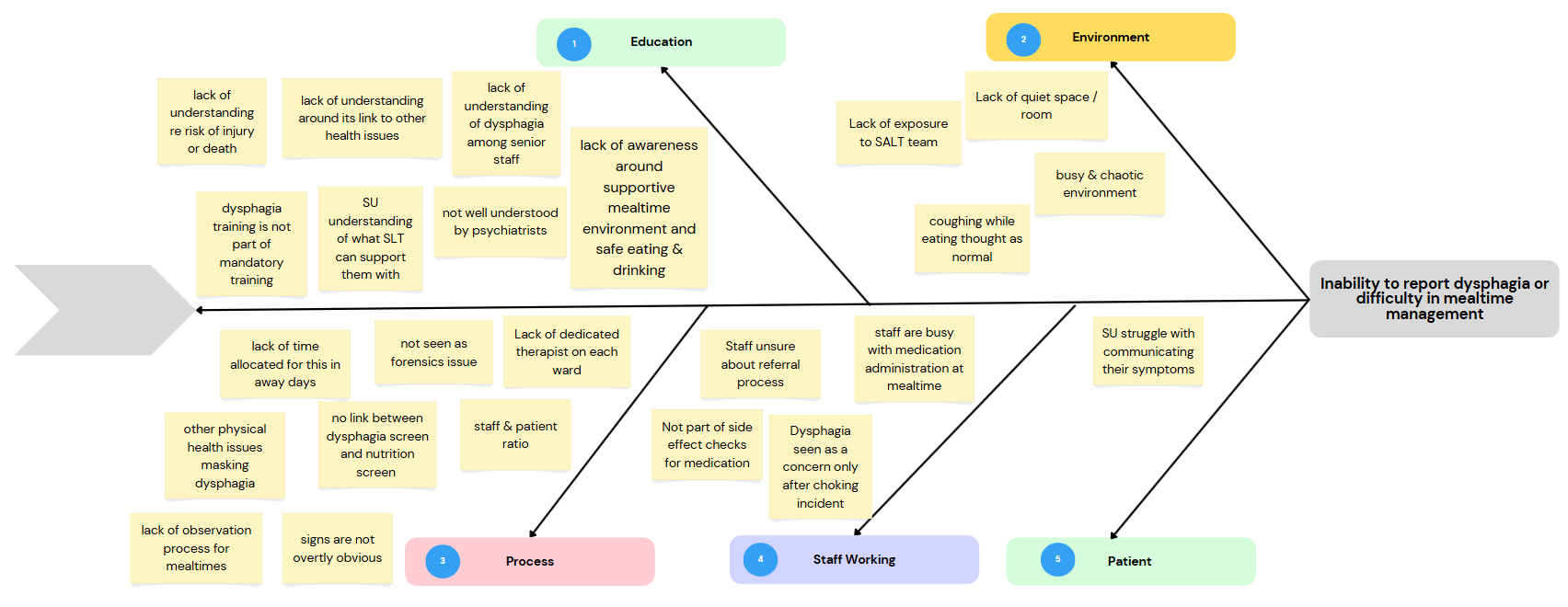
We consulted with service users using easy read materials, a questionnaire and 1:1 interview. We joined away days for several wards and held focused group sessions together with physical health nurses, SALT team, and a trust wide Allied Health Profession (AHP) learning awareness event. We explored the problem that led us to creating a fishbone diagram, as seen in Figure 1.
Figure 1. Fishbone Diagram
The aim of the project was to increase monthly referrals from 0 to 2 referrals for swallowing difficulties in our forensic inpatient services by January 2025.
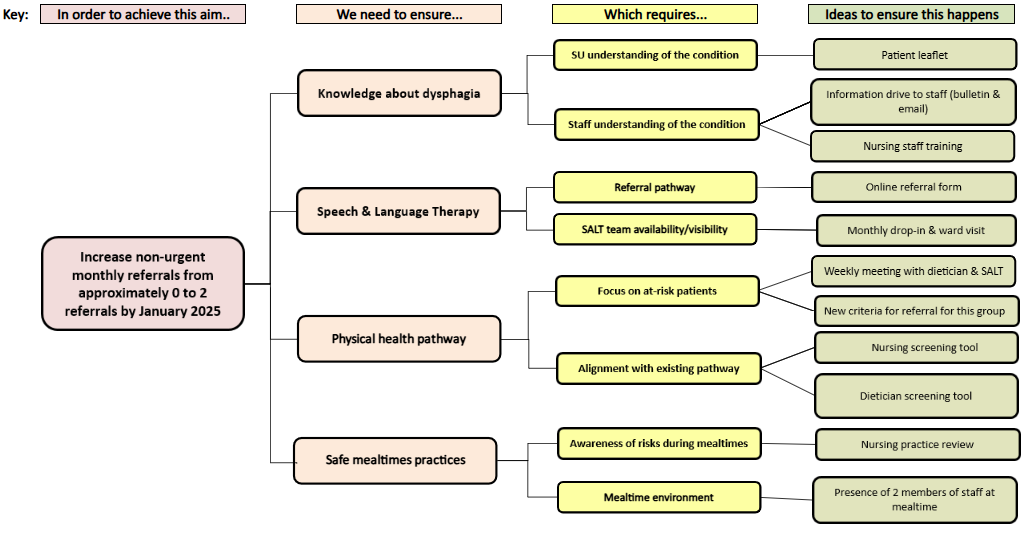
The team created a driver diagram, which was a key part in the process, helping us to consolidate views gathered from different stakeholders. The driver diagram allowed us to organise ideas and breakdown complex information into driving themes and change ideas. Figure 2 below shows the driver diagram with aim, primary drivers, secondary drivers and change ideas.
Figure 2. Driver Diagram
Using Plan Do Study Act (PDSA) cycles, we tested some of these change ideas:
- Physical health checklist including a question about swallowing for nursing assessment (nursing screening tool)
- Audit of patient nutrition & hydration screenings by dieticians (dietician screening tool)
- Regular training sessions offered by SALT as part of physical health team offer
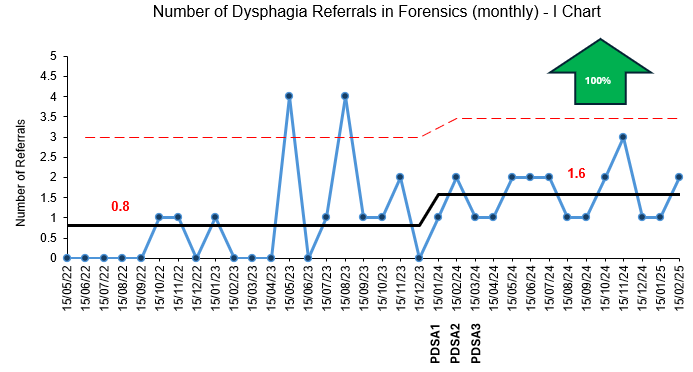
Figure 3. Monthly referrals to SALT team
These change ideas have contributed towards improvement in referral rates (see Figure 3) with a 100% increase in referrals received since the first change idea was introduced. A trial of screening tools used by ward nurses and auditing of screens completed by dieticians prompted discussions around patient swallowing abilities and risks, which consequently increased referrals to SALT team. The training sessions further improved awareness and made the referral process clearer. We learnt that a big proportion of nursing staff were not confident in making referrals to SALT, which we were able to address through a series of training sessions. Figure 4 represents the percentage of staff who felt confident in completing referrals to SALT before and after training between May and July. Feedback showed that they have improved understanding of medication side effects, risks associated with mealtimes in seclusion and the role of their ward SALT team.
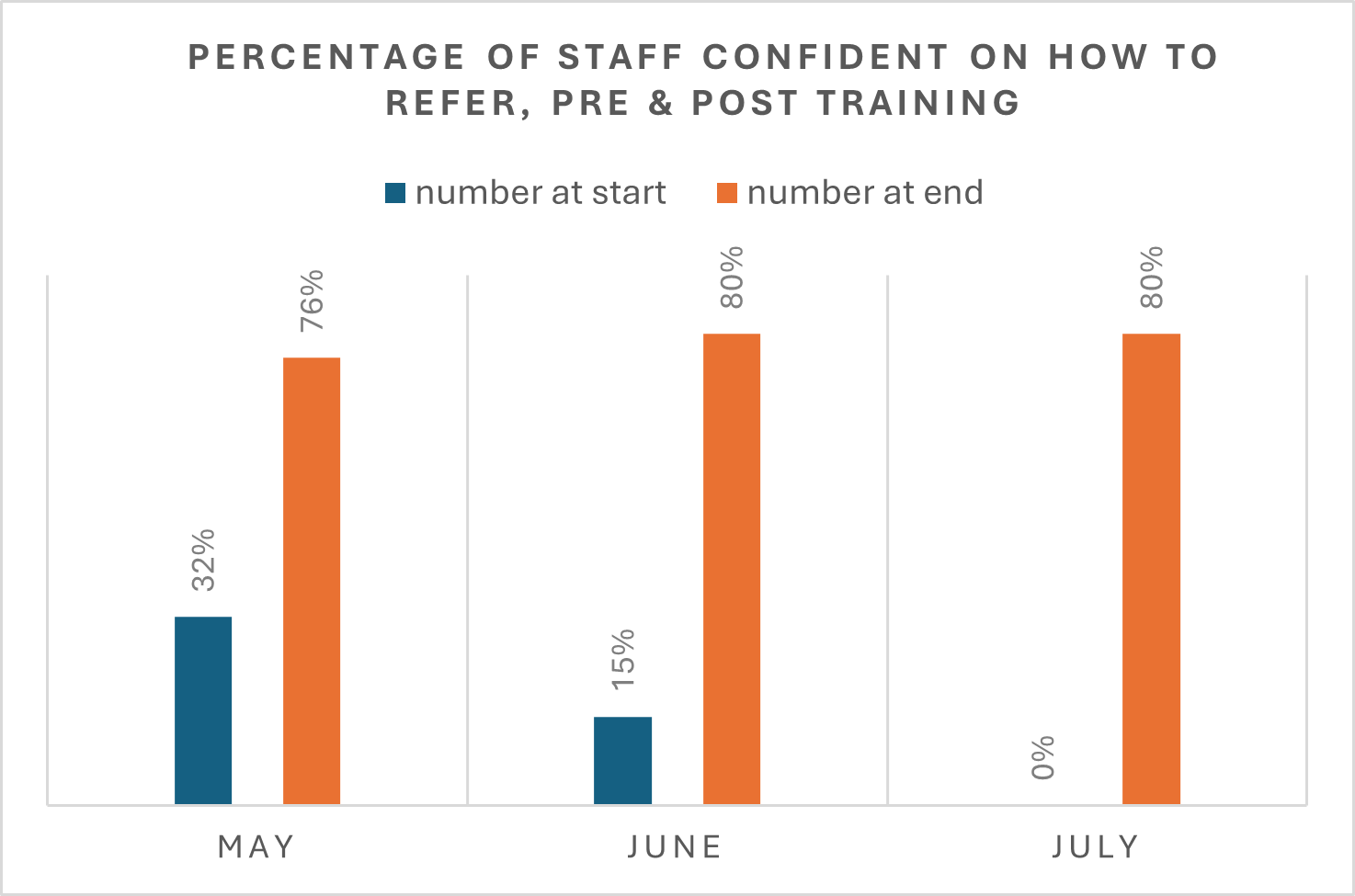
Figure 4. Percentage of staff level of confidence pre and post training in 2024
Severe choking incidents occur more frequently than we thought due to under-reporting of these incidents across the directorate. During the entire project, a serious choking incident was reported via inPhase, approximately every 6 weeks. We felt that regular training in place and discussions around these incidents would address under-reporting.
Overall, this QI project helped us to:
- better understand patient views of our service delivery
- realise “dysphagia” is jargon
- improve accessibility to all stakeholders – even changing our project title, from “early identification of dysphagia within forensic inpatient services” to “making mealtimes safe and comfortable”.
- raise awareness of the often under-estimated and misunderstood risks associated with mealtime difficulties
- train colleagues and increase service visibility
- change our practice and SALT service priorities
Now we are moving forward with the implementation stage and hope to sustain change, with continued training provision, developing a training schedule and offering new admission screens. We would like to pick up other change ideas that came up along the way one day! We are keen to share learning from our project and have had the pleasure of sharing our work at ELFT AHP conference and Forensic QI Forum. The team would also share learnings and results to the directorate management team, across our forensic wards and to other ELFT mental health wards.
Please get in touch at jena.hall@nhs.net if you would like to find out more about this project or to talk about dysphagia in mental health.
To learn more, visit https://www.rcslt.org/speech-and-language-therapy/clinical-information/mental-health-adults/
Reference
RCSLT Northern Ireland. (2023). Adult mental health and speech & language therapy fact sheet. Northern Ireland: Royal College of Speech and Language Therapists. https://www.rcslt.org/wp-content/uploads/2023/02/mental-health-northern-ireland-factsheet.pdf
Most Read Stories
-
Why is Quality Control important?
18th July 2018

-
An Illustrated Guide to Quality Improvement
20th May 2019

-
2016 QI Conference Poster Presentations
22nd March 2016
-
Recognising Racism: Using QI to Help Take Action
21st January 2021

-
Using data enabled us to understand our problem
31st March 2023

-
QI Essentials: What does a Chief Quality Officer do?
18th March 2019


Follow QI on social media
To keep up to date on the latest concerning QI at ELFT, follow us on our socials.