Optimising flow through Ruby Triage Ward
6th March 2025
By Zahra Dwyer (Mental Health Nurse) & Cassie Philpin (Senior Improvement Advisor)
Ruby Ward is a 15 bed, male triage ward based at the Newham Centre for Mental Health where patients are initially admitted for assessment to determine the most appropriate level of care. Following assessment and the early initiation of a care plan, patients are either discharged to the community or transferred to an acute ward for on-going inpatient care.
The intended length of stay on Ruby Ward is 10 days. To support this, all patients have a full mental health assessment and co-produced treatment plan within the first 24 hours of admission and the Multi-Disciplinary Team meet twice daily to ensure plans are progressing.
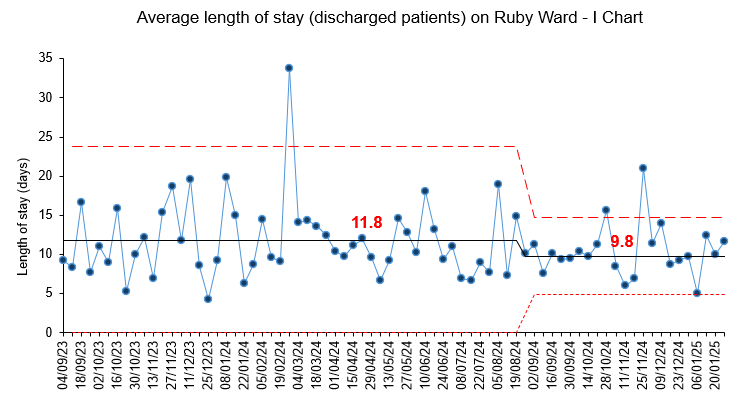
However, data available on PowerBI showed that the average length of stay of patients being discharged to the community was nearly 12 days. So, the ward started a Quality Improvement projects with the aim of improving the flow of patients through the ward.
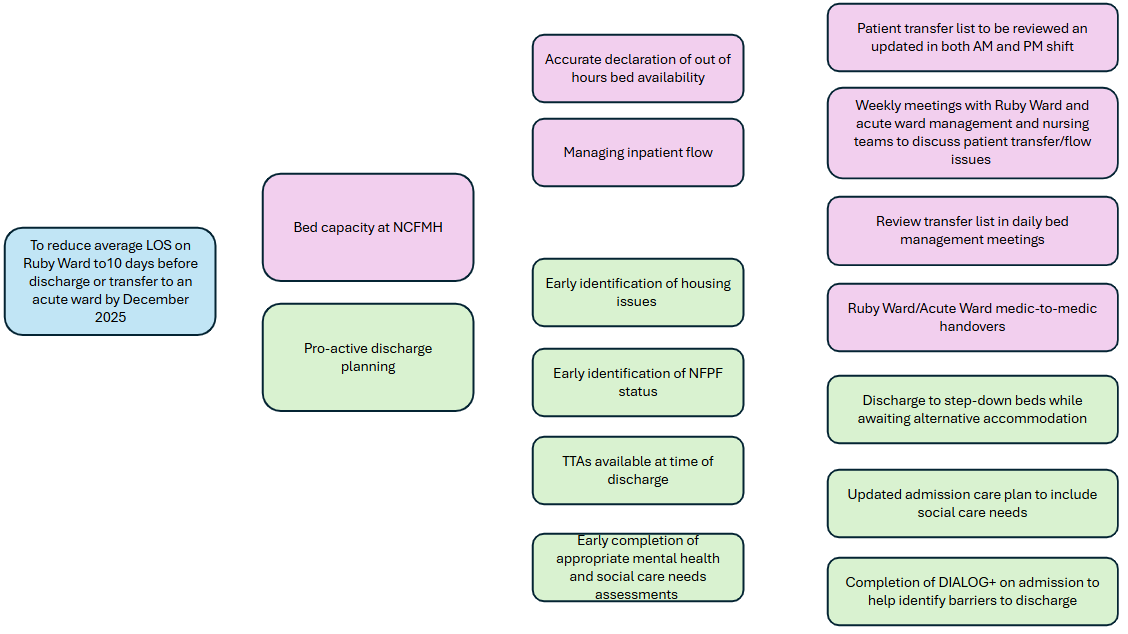
The team used a Driver Diagram (see figure 1) to break down this complex problem into workable change ideas. They identified two Primary Drivers that are required to ensure that the system supports people to step-up or down to the appropriate level of care.
- Proactive discharge planning so that barriers to people returning home are identified and acted upon as soon as possible
- Processes being in place to effectively manage bed capacity at Newham Centre for Mental Health to avoid delays in patients who require on-going inpatient care from being transferred to an acute ward
Figure 1: Driver Diagram
The ward has seen a reduction in the average length of stay for patients who are discharged to the community from 11.8 days to 9.8 days (see figure 2).
Figure 2: Average Length of Stay
Two key changes helped to account for this reduction.
1. The introduction of step-down beds
It is common for patients to be clinically ready for discharge but unable to leave the ward due to a lack of appropriate accommodation. A 10-bed step down service, providing short-term transitional support and accommodation has meant that there is an alternative to people remaining on the ward awaiting social care packages and accommodation.
2. The use of Dialog+
Dialog+ is a patient reported outcome measure which includes questions about the persons satisfaction with different aspects of their life including their work, accommodation, relationships and practical support. Completing this scale with people helps the team to identify potential barriers to discharge so that they can work with patients and other services to overcome them.
When barriers are identified, the ward complete a housing application at the early stages of admission to ensure the necessary documents are gathered for liaising with the hospital housing officer. Communication with the housing services has been improved by attending the ‘bed management’ meeting which occurs every Thursday which enables in-person discussion about discharge plans.
What’s next?
The team think the process of identifying and managing barriers to discharge could be better embedded into routine practice by being included in admission documentation. They have re-designed the admission care plan to include a section on social care needs, in particular the identification of people who require support with legal status, finances and housing. The first test of this change idea is currently in progress using a Plan, Do, Study, Act cycle.
While the reduction in length of stay for patients who are discharged to the community, this cohort of patients only account for about half of all admissions to the ward. So, they are now starting to focus on the other driver of flow through the ward: the ability to transfer patients who require on-going care to acute wards without unnecessary delays.
They have started collecting baseline data on the number of patients who are transferred to an acute ward each week and the time from being identified as suitable for transfer, to being admitted to an acute ward. They will then be testing change ideas which focus on improving communication and planning with the acute wards:
- An improved transfer list to include a section on why transfer to acute ward is required
- Weekly meetings with management and acute ward leadership to review the transfer list
Taking a QI approach to this complex challenge has helped the team break it down into smaller, achievable steps that are gradually helping them improve flow through the system and improve the experience and outcomes of their patients.
Most Read Stories
-
Why is Quality Control important?
18th July 2018

-
An Illustrated Guide to Quality Improvement
20th May 2019

-
2016 QI Conference Poster Presentations
22nd March 2016
-
Recognising Racism: Using QI to Help Take Action
21st January 2021

-
Using data enabled us to understand our problem
31st March 2023

-
QI Essentials: What does a Chief Quality Officer do?
18th March 2019


Follow QI on social media
To keep up to date on the latest concerning QI at ELFT, follow us on our socials.