
Pharmacy involvement in QI: Optimising Diabetes Care through Quality Improvement
6th March 2025
Interviewer: Carlos Santos (Improvement Advisor)
Interviewee: Gogo Abbey (MPharm, Dip.CLinPharm, Independent Prescriber)
🩺 Pharmacists are increasingly shaping the landscape of diabetes management. But what does that look like in practice? I sat down with Gogo Abbey, a clinical pharmacist leading a Quality Improvement (QI) initiative at Cauldwell Medical Centre, to discuss how pharmacists, alongside a multidisciplinary team (MDT) of GPs, nurses, and service users, can work together to co-design better diabetes care.
Gogo is also part of the current wave of ELFT’s Improvement Leaders Programme (ILP), where he has been developing the skills to lead change, test innovations, and embed improvement into everyday practice. His work on this diabetes project is a testament to how pharmacists can collaborate within interdisciplinary teams to apply QI methodology to clinical challenges with real impact.
📖 Glossary (Key Terms Used in This Interview)
💉 T2DM (Type 2 Diabetes Mellitus) → A condition where the body becomes resistant to insulin or doesn’t produce enough, leading to high blood sugar levels.
🩸 HbA1c levels → A measure of average blood sugar levels over the past 2-3 months. Higher HbA1c indicates poorer diabetes control.
⚠ ≥ 58 mmol/mol (HbA1c Threshold for Concern) → When a patient’s HbA1c is 58 mmol/mol or higher, their diabetes is considered poorly controlled, increasing the risk of complications.
💊 Advanced Treatment Options → When diet, exercise, and first-line medications (like metformin) are not enough, patients may need additional interventions to help control blood sugar.
🔎 Identifying the Problem: The Diabetes Challenge
Carlos: What was the key challenge in diabetes management?
Gogo: We had far too many missed diagnoses, delays in treatment escalation, and inconsistent follow-ups. Over 50% of patients with T2DM had an HbA1c ≥ 58 mmol/mol, meaning their diabetes was poorly controlled.
🧠 Understanding the Root Causes
Carlos: Once you identified the issue, how did you deepen your understanding of it?
Gogo: We structured our investigation mapping out the key factors contributing to poor diabetes outcomes. This helped us break down the problem into three main areas:
- 📉 Process gaps → No standard protocol for escalating treatment, unclear referral pathways, and delayed follow-ups for high-risk patients.
- 💊 Limited pharmacist involvement → Pharmacists weren’t routinely consulted in medication escalation decisions.
- 📊 Data limitations → No automated alerts for high HbA1c levels, meaning follow-ups still rely on manual tracking rather than real-time interventions.
- 🗣 Patient engagement barriers → Many patients didn’t understand the importance of follow-ups, and language barriers made effective communication harder.
🚀 Developing a Collaborative Strategy
Carlos: How did you turn this into an action plan?
Gogo: Using the driver diagram as our foundation, we have been designing a co-produced strategy, focusing on:
- 💊 Developing a clear diabetes prescribing pathway → Ensuring patients receive the right treatment at the right time.
- 📢 Improving patient engagement → Translating HbA1c test reminders into multiple languages to increase follow-ups.
- 📊 Using real-time data for better decision-making → Introducing Accurx messaging for high HbA1c alerts.
- 👨⚕️ Upskilling the wider team → Running clinical sessions for GPs and nurses to improve evidence-based medication adjustments.
⚡ Testing and Seeing Results
Carlos: What impact have these changes had so far?
Gogo: We’ve already seen significant improvements:
📉 9% reduction in poorly controlled diabetes cases → More patients now have their HbA1c in a safer range.
💡 Faster medication optimisation → Patients are moving onto the right therapy sooner, reducing the risk of complications.
🗣 Better engagement → More patients are returning for follow-ups thanks to improved communication.
👩⚕️ Stronger integration of the MDT → GPs, nurses and pharmacists collaborate more closely, playing a bigger role in clinical decision-making.
This demonstrates that when the entire MDT—including service users—works together, QI efforts become more impactful and sustainable.
🌱 Sustaining the Gains: The Future of Pharmacy in Diabetes Care
Carlos: Where do you see the role of pharmacists in diabetes care evolving from here?
Gogo: The future of pharmacy in diabetes management will be driven by:
📊 AI-Driven Medicines Optimisation → Using predictive analytics to flag high-risk patients before HbA1c levels spike.
🏥 Expanded Scope for Pharmacist Independent Prescribers (PIPs) → Making pharmacists the first-line prescribers for diabetes medication management to reduce pressure on GPs.
🛠 QI Integration into Everyday Pharmacy Practice → Moving from ad-hoc medication reviews to a continuous improvement cycle that tracks real-time patient outcomes.
📢 Join the IHI Visit to ELFT Pharmacy 2025!
🚀 On 8th May 12:00-13:00, the ELFT Pharmacy team will host its very own IHI Visit —an opportunity to come together, celebrate our achievements, and tackle some of our biggest challenges head-on!
🔍 What’s in it for you?
- ✅ Learn how pharmacists can drive large-scale improvement projects.
- ✅ See real-world applications of QI methodology in medicines optimisation.
- ✅ Network with leading pharmacy innovators in the NHS & IHI community.
🔗 Spots are limited—register now!
Most Read Stories
-
Why is Quality Control important?
18th July 2018

-
An Illustrated Guide to Quality Improvement
20th May 2019
-
2016 QI Conference Poster Presentations
22nd March 2016
-
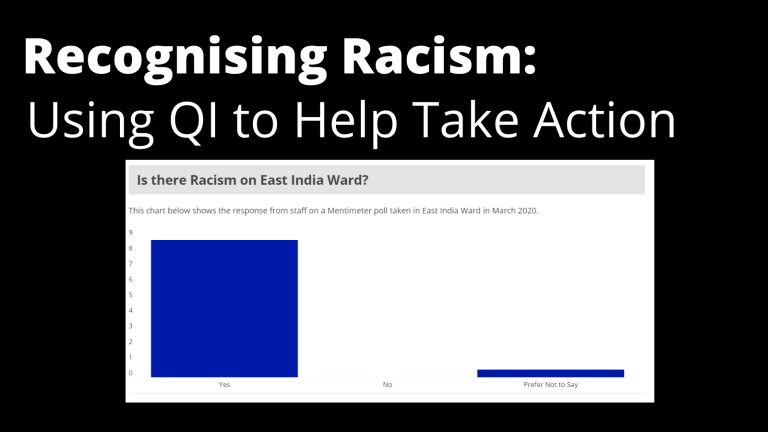
Recognising Racism: Using QI to Help Take Action
21st January 2021
-
Using data enabled us to understand our problem
31st March 2023
-
QI Essentials: What does a Chief Quality Officer do?
18th March 2019

Follow QI on social media
To keep up to date on the latest concerning QI at ELFT, follow us on our socials.


