Preventable Pain: Reducing Catheter Blockages for Tower Hamlets Residents
17th February 2025
Written by: Ayodele Ajibade (Clinical Lead), Shanaz Basit (Service User), and Clarissa Sørlie (Improvement Advisor)
Catheter blockages are a preventable problem, yet they continue to cause pain and distress for patients. To address this, the Tower Hamlets Rapid Response team launched a Quality Improvement (QI) project that is already making a significant impact. Since October 2024, there has been a 22% reduction in people experiencing problems with their catheters – from 29.4 to 22.8 per week. Not only has this improved patient experience but has also freed up 40 hours of staff time per month, allowing the team to provide urgent care more quickly to other patients. This equates to an estimated saving of £1,155.53 each month in staff time. Additionally, because staff travel to patients’ homes, this is estimated to reduce carbon emissions from car journeys by at least 236.8kg per year.
Why do catheter blockages matter?
Imagine: you wake up in excruciating pain. You suddenly remember that you have a catheter, a small tube that empties your bladder into a drainage bag. A wave of panic grips you. You realise that your catheter could be blocked. Your urine has nowhere to go. Your bladder stretches past its limit. As the pressure mounts, you know that you are at risk of kidney damage and infection if you don’t get help quickly.
Each year, 15-25% of patients admitted to NHS hospitals require catheterisation (Health Economics Research Unit, 2015) and over 90,000 people in the community in England rely on long-term catheters (Gage et al., 2017). Catheters are inserted for a range of reasons, including when people are having difficulty urinating naturally or to improve comfort for people who are terminally ill (Barrie, 2025). However, blockages are a common risk, affecting between 20-70% of catheters (Paterson et al., 2019).
This is where the Tower Hamlets Rapid Response team come in. The team visit people in their own homes and provide urgent assessment and treatment to prevent hospital admissions. Between May and September 2024, the team responded to an average of 29 calls a week for catheter-related problems such as blockages or leaking (often a symptom of a blockage or problem with the catheter).
Starting a QI project
Reducing catheter blockages isn’t about individual care, it’s about a culture shift. The Tower Hamlets Rapid Response team knew this, and saw the opportunity to move away from reactive, crisis-driven responses towards a culture where catheter problems are prevented.
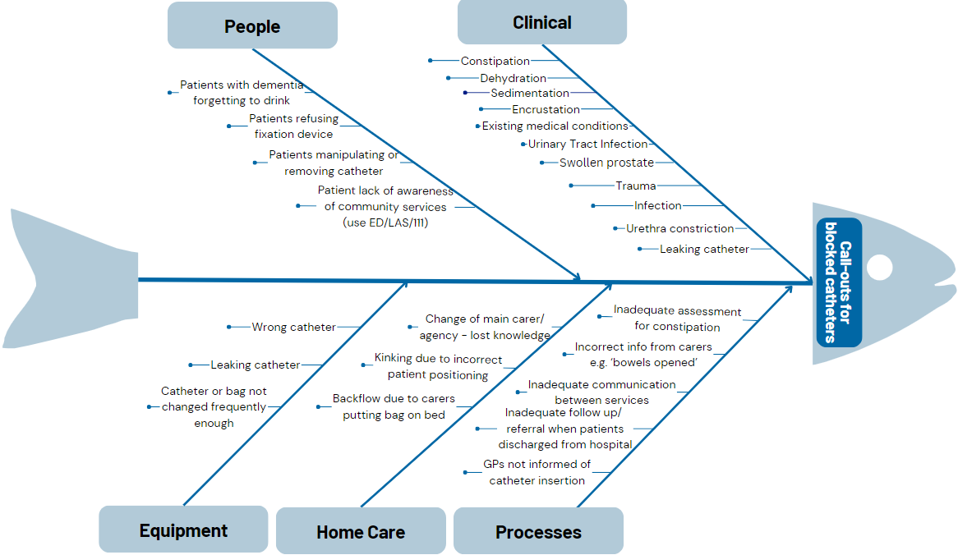
Led by Ayodele Ajibade (clinical lead), the team pooled their collective knowledge and expertise about the causes of catheter blockages into a Fishbone Diagram (see Figure 1).
Figure 1. Fishbone diagram for the causes of blocked catheters
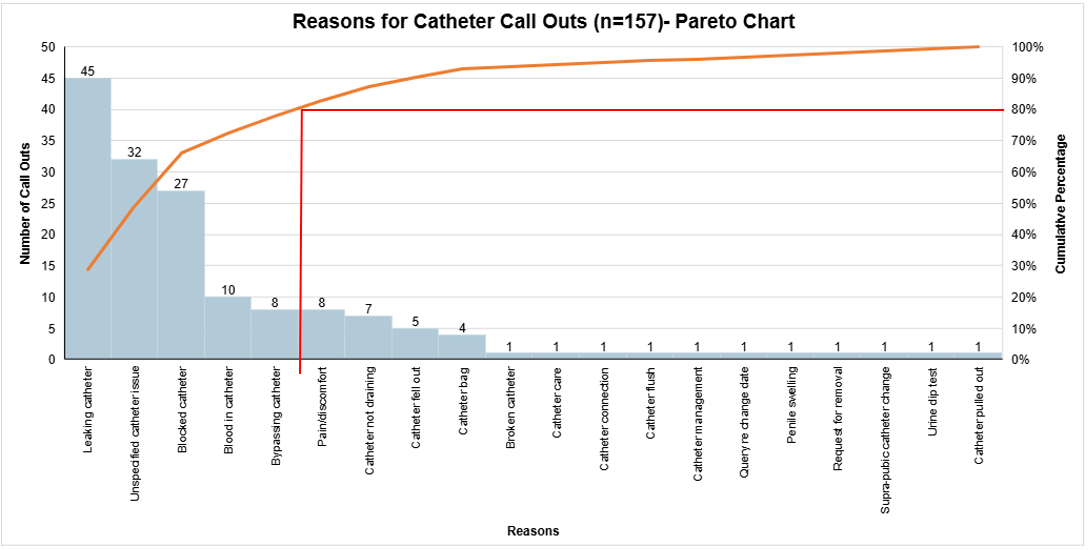
Over the course of five weeks, the team recorded the reason for every catheter-related call that they received – 157 calls in total. By organising this data into a Pareto Chart, the team were able to see that blocked catheters accounted were the third highest reason for catheter call-outs (see Figure 2).
Figure 2. Pareto Chart for reasons for catheter call outs
Change Ideas
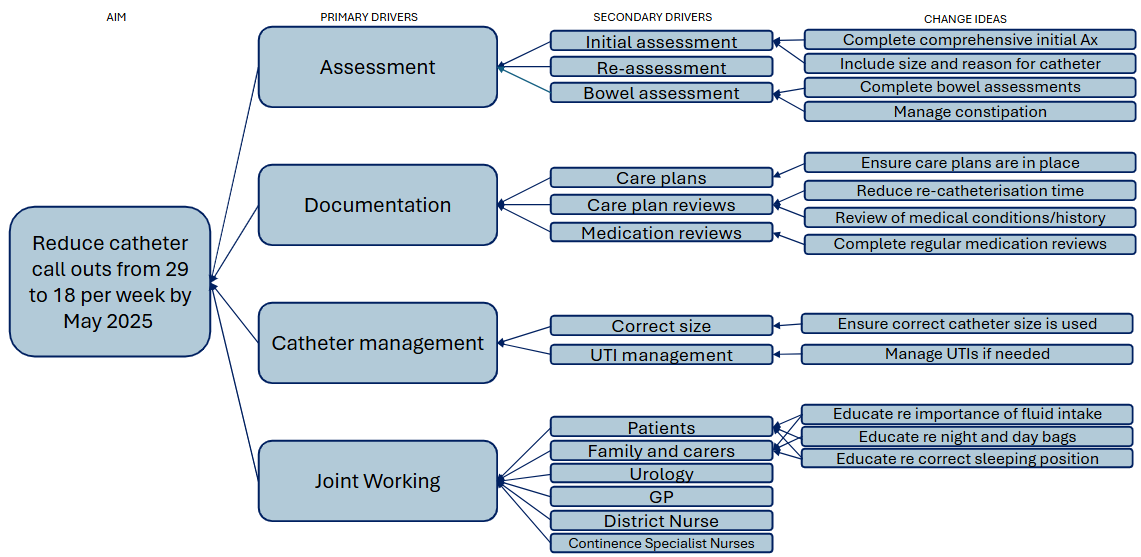
The team generated change ideas about how to improve catheter care, which they organised into a driver diagram. This tool helped the team to communicate their theory of what needs to change in the current system to lead to an improvement (Bennett and Provost, 2015).
Figure 3. Driver diagram illustrating the team’s theory of change
So far, the team have tested the following change ideas:
- Identifying patients whose catheters block frequently and developing individualised plans for each patient, targeting the cause of the blockage
- Re-assessing the need for catheters for patients whose catheters are frequently expelled
- Introducing consistent constipation assessments
- Gaining specialist advice on the management of complex cases from the Barts Health Bladder and Bowel Specialist Nurse Practitioner
Outcomes
Despite the project still being in early stages of testing, the team has already started to see an improvement. Weekly call outs have reduced from 29.4 to 22.8 (see Figure 4), which is equivalent to approximately 40 hours of staff time. This leads to an estimated monthly saving of £1,155.53 in staff time (see Figure 5).
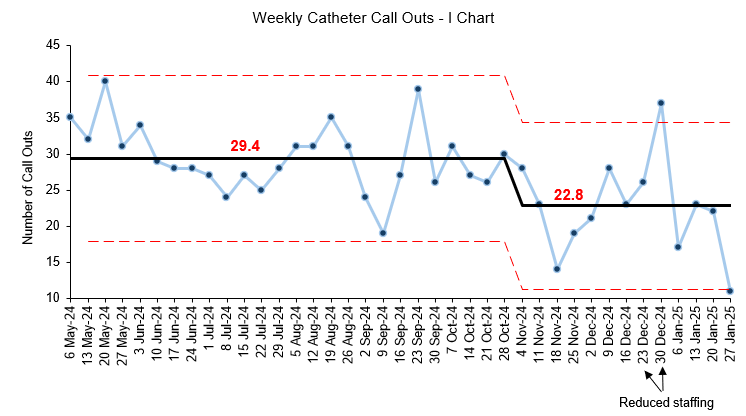
Figure 4. Control chart showing a reduction in catheter call-outs
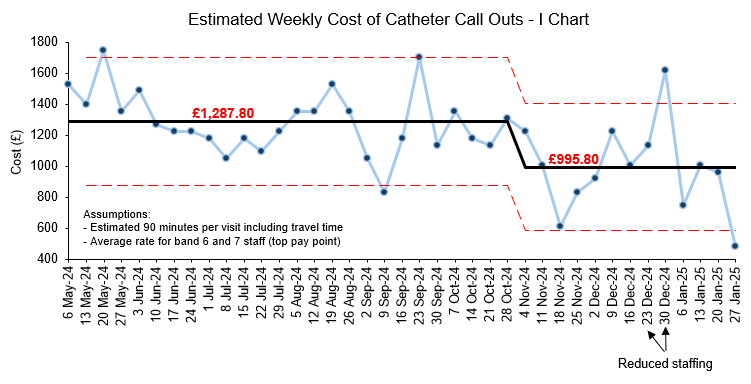
Figure 5. Control chart showing a reduction in weekly cost of catheter call outs
Additionally, a reduction in visits equates to a 236.8kg carbon saving per year based on an average round-trip car journey of nine miles. That’s enough to charge 19,145 smartphones (United States Environmental Protection Agency, 2025).
Reflecting on the impact of this work, project lead Ayodele Ajibade said, “This project is improving the quality of life for patients and their families. It also saves costs and releases health professionals (like paramedics, care staff, community nurses and hospital staff) to attend to other clinical priorities.”
Tackling this complex problem will need continuous learning and persistence. Although the initial results are promising, the team knows their work isn’t finished. They are committed to testing and refining more change ideas in their pursuit to prevent catheter blockages before they impact patients.
To learn more about the work of the Rapid Response team, listen to their podcast episode or visit their information page on the ELFT website.
References:
Barrie, M. (2025) ‘An Overview of the Cost and Complications of Catheterisation’, Urology and Continence Care Today [Online]. Available at: https://www.ucc-today.com/journals/issue/launch-edition/article/an-overview-of-the-cost-and-complications-of-catheterisation (Accessed: 12th February 2025)
Bennett, B. and Provost, L. (2015) What’s Your Theory? [Online]. Available at: https://qi.elft.nhs.uk/resource/whats-your-theory-2 (Accessed: 12th February 2025)
Gage, H., Avery, M., Flannery, C., Williams, P. and Fader, M. (2017) ‘Community prevalence of long-term urinary catheters use in England’, Neurology and Urodynamics, 36(2), pp. 293-206. DOI: 10.1002/nau.22961
Health Economics Research Unit (2015) Reducing Hospital Infections: Which Catheter? [Online]. Available at: https://www.abdn.ac.uk/media/site/heru/documents/HERU_PB_December_2015.pdf (Accessed: 12th February 2025)
Paterson, C., Dalziell, R., Forshaw, T., Turner, A. and Frasher, G. (2019) ‘Prevention and Management of Urinary Catheter Blockages in Community Settings’, Nursing Standard, DOI: 10.7748/ns.2019.e11431
United States Environmental Protection Agency (2025) Greenhouse Gas Equivalencies Calculator [Online]. Available at: https://www.epa.gov/energy/greenhouse-gas-equivalencies-calculator (Accessed: 12th February 2025)
Most Read Stories
-
Why is Quality Control important?
18th July 2018

-
An Illustrated Guide to Quality Improvement
20th May 2019

-
2016 QI Conference Poster Presentations
22nd March 2016
-
Recognising Racism: Using QI to Help Take Action
21st January 2021

-
Using data enabled us to understand our problem
31st March 2023

-
QI Essentials: What does a Chief Quality Officer do?
18th March 2019


Follow QI on social media
To keep up to date on the latest concerning QI at ELFT, follow us on our socials.