
Tower Hamlet’s ‘Making People Better’ programme
19th December 2013
by Dr Nick Bass
Why do you come to work? Are you proud of what you do? Would the service you provide meet the standards you require for your own friends and family?
Despite all the effort and time we put into our work, if the answer to the above is that there is ever anything about the service we deliver that could or should be done better that means there is an opportunity – or obligation even – for Quality Improvement. The purpose of this programme is to enable anyone and everyone with a responsibility for the service (clinical, non-clinical, managerial, support services) and those who make use of the service (patients) and their carers to contribute directly to that improvement. It is about going further than identifying problems but in trying to come up with solutions to those problems – problems that staff and patients experience as priorities and which staff and patients are best placed to try and fix.
Everyone with a role to play in the wider health service (including those who experience the delivery of this service) is invited to attend a ‘Making People Better’ afternoon which introduces the concept of QI and also gives everyone an opportunity to air their own priority concerns and try and find solutions to those problems.
So far, at least half the attendees have found a solution to their problems and many of the others have found a way to try and resolve theirs. This can be done in a surprisingly short time. The principles are grounded in cognitive psychology though the actual delivery is deceptively simple.
QI can be about changing the way organisations work from the top down and a number of well-known approaches have arisen in non-health industries but which have been applied to health organisations in the UK and abroad with varying degrees of success (such as ‘Lean’ at Toyota and ‘Six Sigma’). But some of the most effective approaches to QI have come from ‘coal-face’ staff and patients. BMJ Publishing has developed electronic QI workbooks to support teams and has found significant success in low-literacy areas of Low and Middle-Income countries as well as with more complex projects in the UK and Europe. Our own experience of working in resource-poor settings such as Uganda and Somaliland has demonstrated the incredible health gains which can be achieved by simply engaging staff, patients and families and enabling them to take some control of decisions and how services are developed and delivered.
There will inevitably be tensions surrounding the successful implementation of QI. We all want services which are safe and effective but they also need to be efficient/cost-effective. These frequently run counter-current to each other. It may be tempting to simply take an axe to ‘red-tape’ and bureaucracy but care needs to be taken not to dispense with useful safeguards when trying to get rid of policy barriers to improvement. And organisations know that good practice may only occur in isolation – but that rolling it out uniformly as policy removes the local ownership which made it effective in the first place.
Our Trust has identified violence on wards, suicide by CMHT patients and improving the patient experience as its top 3 priorities. But how can an organisation square the circle? On the one hand these major priorities which need addressing everywhere and with some consistency of outcomes; on the other the recognition that problems are most effectively addressed with local solutions. A central or federal approach?
The Tower Hamlets Making People Better programme may offer a way of doing just this. Handing control of serious health issues to local services and teams (simple problems such as the spread of infection and hand-washing, or complex problems such as cystic fibrosis management) has been shown to be profoundly effective. But already some local initiatives have shown how local engagement and ownership can also make a significant positive impact on mental health priorities (a simple programme for violence reduction on the wards; a far more complex training programme to reduce the impact and frequency of Serious Incidents).
Cultures do not change overnight and are said to need at least a generation. But that seems to depend on external or top-down pressure. If people want to make changes then things will move much more quickly. Making People Better hopes to do exactly that. There is no promise of solving any particular problem quickly or even at all. The easiest problems will generally be the simplest (but not necessarily) and overall organisational outcome improvements may take time if they depend on hundreds or thousands of such small improvements. But these may compound to help meet ambitious Trust ‘stretch targets’ and, if successful, are far more likely to be sustained over time because people want to maintain the outcomes.
Making People Better is about more than just making our patients better – it is about getting the best out of everyone. The programme seems to be successfully engaging a wide variety of people and a number of initial sceptics have come away with solutions they were not expecting or at least the ideas and resources they might need to find those solutions.
Most Read Stories
-
Why is Quality Control important?
18th July 2018

-
An Illustrated Guide to Quality Improvement
20th May 2019
-
2016 QI Conference Poster Presentations
22nd March 2016
-
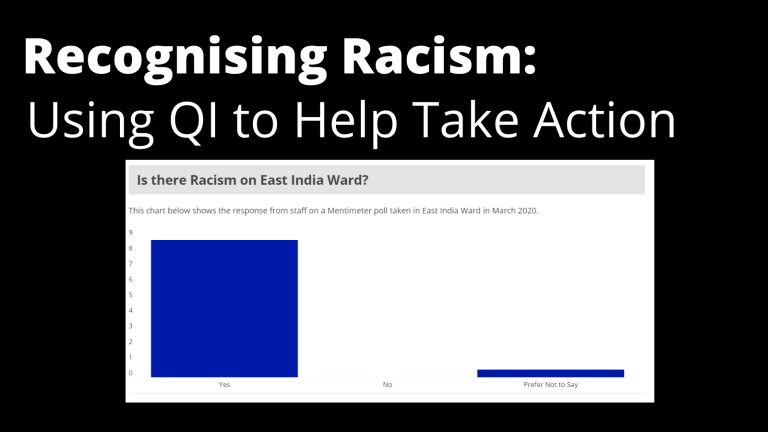
Recognising Racism: Using QI to Help Take Action
21st January 2021
-
Using data enabled us to understand our problem
31st March 2023
-
QI Essentials: What does a Chief Quality Officer do?
18th March 2019

Follow QI on social media
To keep up to date on the latest concerning QI at ELFT, follow us on our socials.



