
Using QI To Manage A Huge Increase In Demand
29th September 2021
By Nicola Ballingall, Improvement Advisor
In this 10 min read, learn about how one of our Primary Care GP practices in Bedfordshire, Cauldwell Medical Centre, is using quality improvement (QI) to manage the huge increase in demand on their service.
It’s August 2021 and the world is starting to open up again after the pandemic. 98.2% of UK GPs state that the patients they see are presenting with increasingly complex care needs and 90% report experiencing high pressure from increased workloads (PRUComm, 2021). Cauldwell Medical Centre set out to reduce avoidable appointments with GPs from 27% to 0% in 6 months (by November 2021).
Requests to see GPs and Advanced Nurse Practitioners is huge, the surgery haven’t been able to answer all the calls coming in, and clinicians are rushed off their feet, relying on people missing appointments just to get their admin done. Only 72% admin slots were used because staff needed to spend that time with patients and 7 minutes appointment slots were often not long enough. Minaz-Mazi Kotwal (Portfolio GP) describes the problem: “Cauldwell Medical Centre has a very high ethnic diversity, which often means ten minutes consultations are impossible and, even with an interpreter, the twenty minutes consultations last longer than planned. Double appointments for complex patients means fewer patients can be seen and this has a huge impact on our capacity. There is no protected time for when colleagues have queries or a nurse wants a non-duty doctor to review a patient.”
The priority for patients was having face to face time with their clinicians, and many have waited over a year because they did not want to be seen over a video call. One patient said that Cauldwell Medical Centre, “has been good before the pandemic, but I have not been able to see a doctor for over a year to talk about any concerns I have”, and another said, “You have to keep phoning up at 7:55am as most times (the appointments) are gone by 8am.”
Something needed to be done to match the capacity of the staff with this increased demand. So the GPs, nurses and administrators came together to run a demand and capacity QI project. The project lead is Gautham Bagga, lead GP, and is supported by the ELFT QI Department and Time for Care, an NHS body who support Primary Care Networks to improve. The team have had difficulty recruiting a service user to join their project, but Primary Care has two new Patient and Community Engagement Leads whose role will include supporting co-production in QI.
To better understand the problem, the team started by measuring their ABCDs – their Activity, Backlog, Capacity and Demand – in search of bottlenecks, or constraints, as shown in Figure 1.
Figure 1: Measure ABCD at the bottleneck
Demand
Demand includes all requests and resources needed, such as room time, incoming calls and even demand that can’t currently be met. The QI project team broke this down into predictable planned and unplanned demand and unmet demand. The predictable, planned demand included appointments, prescription requests and administrative tasks (as shown in Figure 2); unplanned but predicable care including on the day acute appointments, phone calls and nursing activity, such as dressings; unmet demand including dropped calls and people who were going to A&E instead of the GP surgery.
Figure 2: Tasks: a type of predictable, planned demand – ‘ICDS Diabetes’ means diabetes nurse, this data was collected as a sample for a one week period
Backlog
Then it was time to look at the queue/backlog data, i.e. the mismatch between demand and capacity. This is different from the waiting list as it is unsustainable. Reception staff tallied the number of times a patient was asked to call back because the appointment they needed was not available. This data was tallied for a sample period of 2 weeks, as shown in Figure 3.
Figure 3: A Tally of Call Back Requests (Queue)
The run chart in Figure 4 shows how many GP and Advanced Nurse Practitioner (ANP) appointments were requested and could not be provided. You can see the queue ranges from 1 to 11 people per day, which is not huge for a GP practice, so the team turned instead to look into whether any of the appointments they were providing were avoidable.
Figure 4: Number of Appointments that could not be Provided (Queue) (Run Chart)
Activity
The team took a closer look at the work they were actually doing, called ‘Activity’ (Figure 5). They could see they were using most of their clinic and doctor sessions (circled in green), but to the detriment of not being able to protect the time for admin sessions (circled in red).
Figure 5: Sessions Used (Activity)
The support team counted the number of GP appointments carried out daily by creating the Statistical Process Control chart in Figure 6. They noticed that Mondays tended to be busier and there was special cause variation in the number of appointments after the long easter weekend, which has helped the team to plan for higher demand the week after the August bank holiday.
Number of working day GP appointments (Activity) (C Chart)
Figure 6: Number of working day GP appointments (Activity) – C Chart
Clinicians believed that a significant amount of the appointments they offered were avoidable for one of the following reasons:
- Patient could have been seen by another clinician in the practice
- Need could have been met by another local service
- The demand came from anther organisation
- If the system worked better the need would not have arisen.
Ten GPs ran an avoidable appointment audit and reported that 27% of their appointments were indeed avoidable (Figure 7). This was higher than the national average of 24% (Primary Care Foundation, 2021).
Figure 7: Avoidable Appointment Audit (Activity)
The doctors reflected that the majority of these appointments could have been carried out by another clinician in the practice, which has prompted the team to really utilise the other professionals in their network (Figure 8).
Figure 8: Avoidable Appointment Audit (Activity)
Capacity
Once the team had measured their activity, backlog and demand, they turned to look at their capacity. The group mapped out what resources they had, including equipment and staffing, taking into account sickness and meetings.
They found areas of unused capacity (Figure 9), i.e. work they had scheduled time for that was not required. This included slots for 111 calls, professional contact slots and 40min home visits appointments. Once the team realised this, they were able to plan to use that time to see patients.
Administration tasks were not being handed over when people went on leave. GPs were reading all the incoming letters when this could be done by other professions, and the surgery was not utilising the Primary Care Network professionals available to them, like paramedics, physios, prescribers and care co-ordinators. They discovered that their nursing capacity did not meet the demand, which inspired them to test a new rota with 4 long nursing days.
Figure 9: Slot Types (Capacity)
Process Mapping
To gain a system wide view of all this new intel, the team process mapped the whole patient journey, noting where they had data on demand and capacity as well as gaps in their knowledge. They could see a significant amount of rework in their process for reauthorising prescriptions, so mapped out this process in more details (Figure 10). This generated some change ideas, which they added in hexagonal boxes.
Figure 10: Reauthorisation of Prescriptions Process Map
All this data analysis sparked plenty of ideas for improvement, so it was time to start developing a change strategy. The team are still working on narrowing down their aim as they build their understanding of the data available to them. Currently, the broad aim is “To best manage the demand and capacity at Cauldwell Medical Centre in 7 months (by December 2021)”. The Medical Director led the QI project team through the nominal group technique, where everyone is able to record their change ideas on post-it notes. They then used a prioritisation matrix (Figure 11) to decide which ideas would have the most impact and be easiest to implement.
Figure 11: Prioritisation Matrix
The change ideas were organised into a driver diagram to visualise how they all contribute towards the aim (Figure 12). For example, one of the primary drivers was to standardise key processes, and an associated change idea was to use a code on the appointment system to mark people who require a translator. The team couldn’t wait to get started. They planned to test all the yellow change ideas in the first week … and failed. They realised they needed to plan each one out so that people were clear on their responsibilities.
Figure 12: Driver Diagram
They used the Life QI website to record the Plan, Do, Study, Act (PDSA) phases of their first test of change, which was to utilise those Primary Care Network professionals, ie. paramedics, physiotherapists and care co-ordinators. In the ‘Plan’ phase they agreed who would refer patients, when and how, and they predicted that this would reduce the number of GP appoints by 100 weekly.
The team carried out the ‘Do’ phase at the beginning of July. The support team were successfully trained in non-clinical triaging and they tracked their progress by measuring the number of GP appointments carried out (Figure 13).
Figure 13: Number of GP Appointments carried out (weekly) (C Chart)
In the Study phase people had a sense that more PCN (Primary Care Network) referrals had been made and that the freed-up GP capacity had been used to reduce the queue; it had not reduced the intensity of their day. The number of appointments is now decreasing partly due to offering 60-day prescriptions and party because the surgery have not been able to recruit a full team of GPs.
In the Act phase the practice manager decided to track the number of PCN appointments used and collate this on a run chart so the impact of the next PDSA could be measured.
Since starting the project 5 months ago the team have invested 21 hours into QI meetings and expect to make that time back many times over by matching demand to capacity. They have learned an immense amount about how they can improve patient care and staff satisfaction. This has been made possible because this dedicated team have used QI to tackle what is most important to their service right now. In just 6 months they aim to transform their surgery to become an outstanding place to give and receive care.
Figure 14: QI Project Team
References
PRUComm (2021) 9th National GP Worklife Survey (online)
Primary Care Foundation (2021) Potentially Avoidable Appointment Audit (online)
Most Read Stories
-
Why is Quality Control important?
18th July 2018

-
An Illustrated Guide to Quality Improvement
20th May 2019
-
2016 QI Conference Poster Presentations
22nd March 2016
-
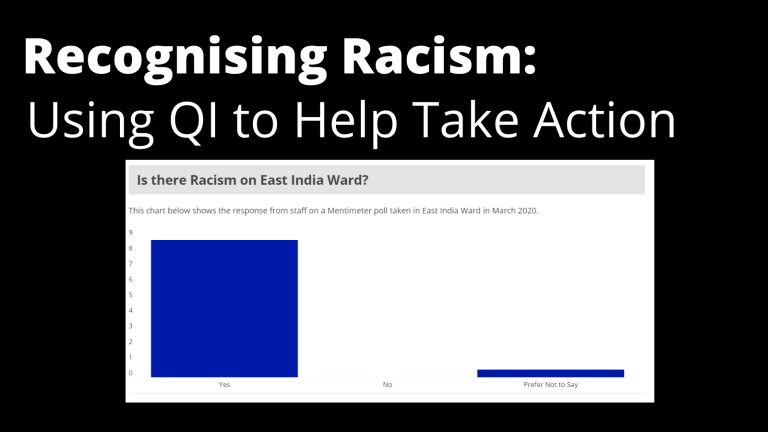
Recognising Racism: Using QI to Help Take Action
21st January 2021
-
Using data enabled us to understand our problem
31st March 2023
-
QI Essentials: What does a Chief Quality Officer do?
18th March 2019

Follow QI on social media
To keep up to date on the latest concerning QI at ELFT, follow us on our socials.




















