Optimising Flow
What is Optimising Flow?
Our growing population and the increasing acuity and complexity of healthcare needs have all contributed to an increase in demand for our services. Our capacity, i.e. the staff and resources available to support our patients, needs to match this demand in order to maintain good quality care. By matching demand and capacity, we can optimise the flow of patients through our systems, i.e. reduce waiting times and improve patient pathways with the resources we have.
In response to these issues, the Trust launched a Quality Improvement (QI) programme to optimise flow.
Phase 1
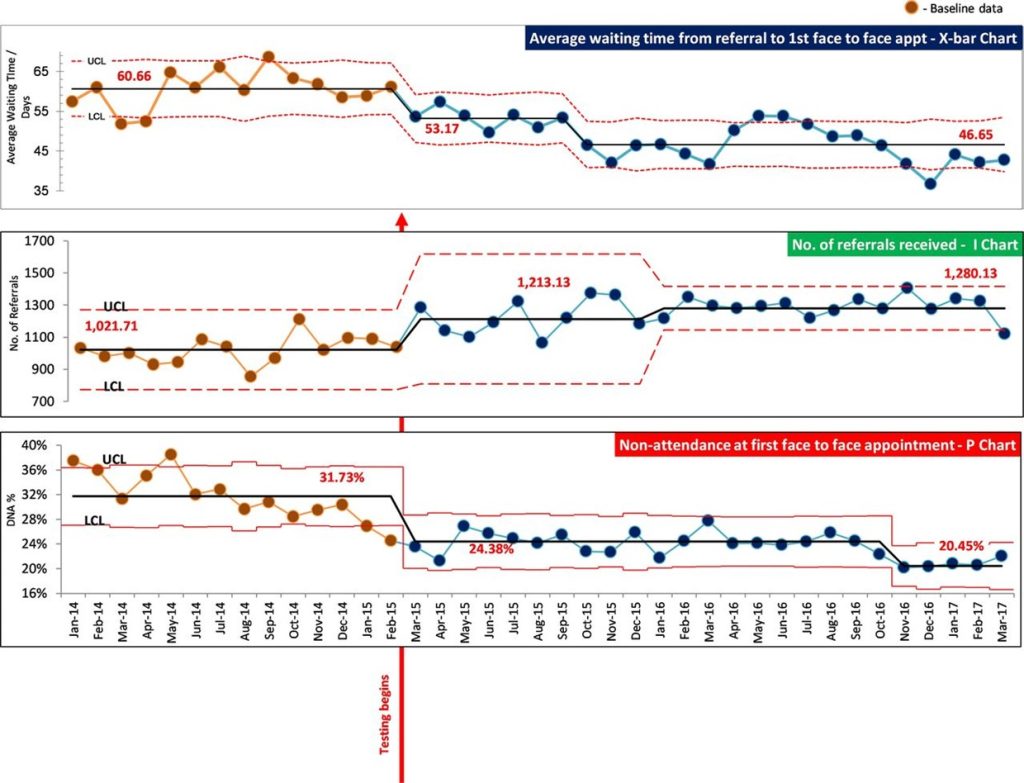
The first phase of the programme ran between 2015 and 2017, with a focus on improving access to community-based services within the Trust, specifically around the following areas:
- Reducing waiting times to first appointment
- Reducing missed appointments
- Increasing new referrals
Fifteen diverse teams including, adult community teams, mental health teams, child and adolescent mental health services, secondary care psychological therapies services, memory services, a musculoskeletal physiotherapy service and a sickle cell service came together in a collaborative learning system supported by the ELFT central QI team.
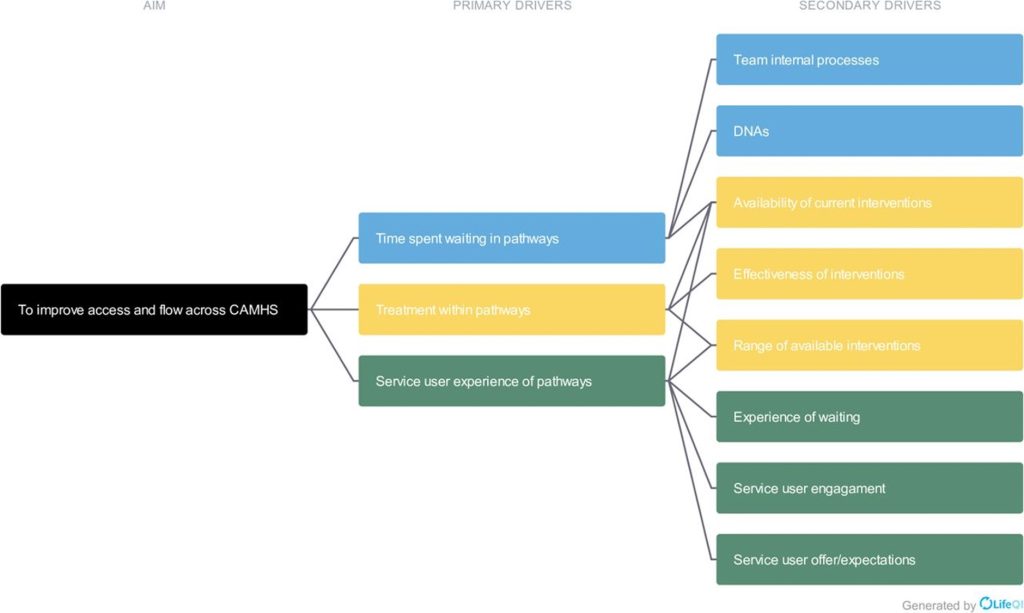
The following figure shows the collaborative’s theory of change.
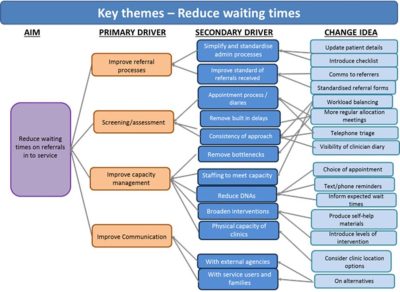
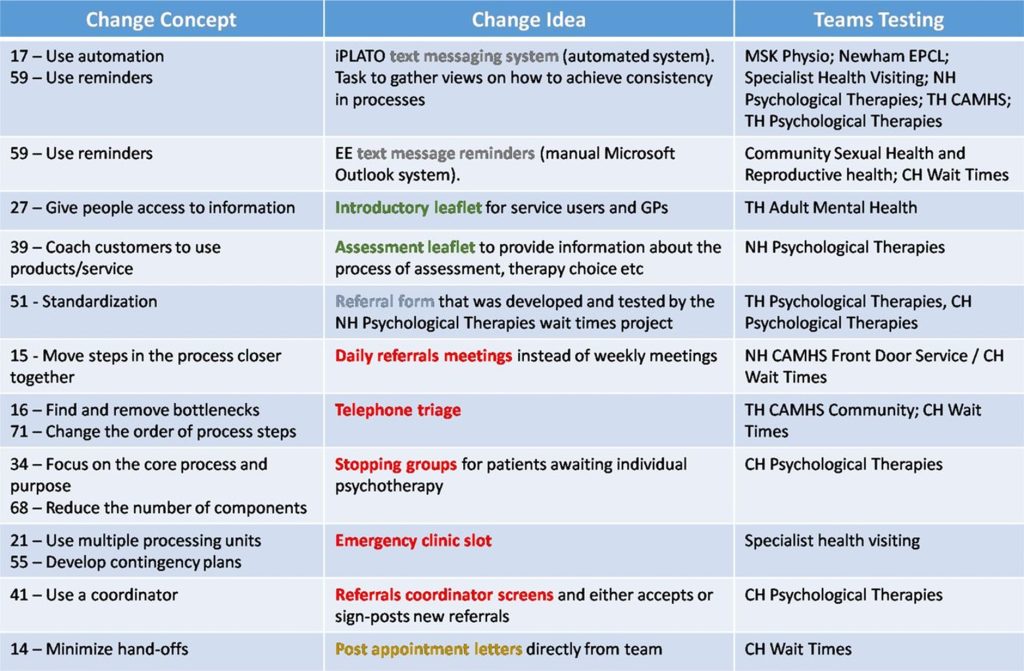
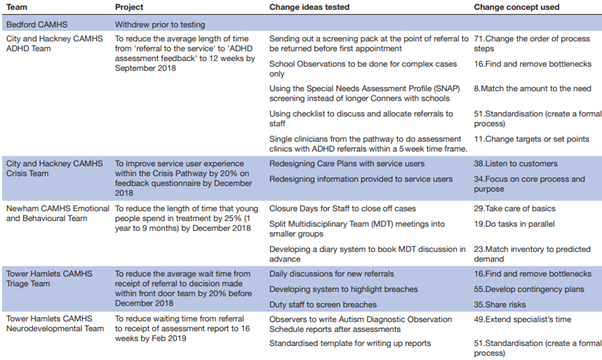
Over two years, the teams tested out a variety of change ideas which are shown in the table below:
The programme achieved significant improvements over the two years:
- The average waiting time from referral to the first face-to-face appointment was reduced from 60.6 days to 46.7 days, a 23% reduction
- Missed appointments at the first appointment dropped from 31.7% to 20.5%, a 36% reduction
- The volume of referrals increased by 25%, from an average of 1021 per month to 1280 per month
Featured Articles
Phase 2
As these teams moved into quality control, Phase Two of the programme was launched in 2017.
The aim of the programme was to reduce waiting times and improve the overall flow of service users through Child and Adolescent Mental Health Services (CAMHS), ensuring timely access to mental health services for children and adolescents.
Seven CAMHS teams from ELFT participated in this collaborative learning system. These teams included interdisciplinary professionals working across different geographical areas within the Trust. The teams came together every six weeks to learn from each other about what was working and what was not.
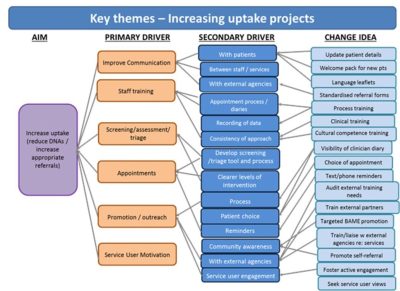
The programme’s theory of change can be seen below:
Across the programme, many change ideas were tested to improve access and flow. A summary of these ideas can be seen in the table below:
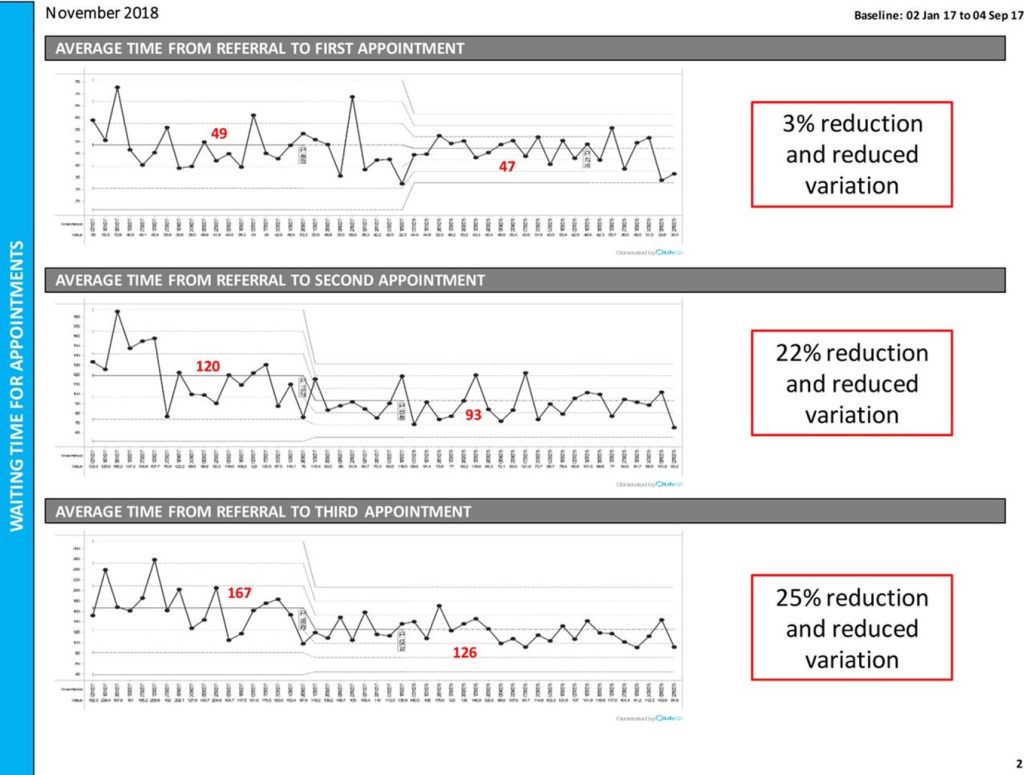
These change ideas resulted in several improvements at both team level and at systems level. Most notably:
- Time from referral to first appointment reduced from an average of 49 days at baseline to 47 days: a 3% reduction
- Time from referral to second appointment reduced from an average of 120 days at baseline to 93 days: a 22% reduction
- Time from referral to third appointment reduced from an average of 167 days at baseline to 126 days: 25% reduction
Phase 3
In the wake of the Covid-19 pandemic, many clinical teams at ELFT faced growing demand for their services and long waiting lists for people to receive the care they needed. In response to this, we launched Phase Three of the programme, which began in early 2021.
This saw over 50 teams across all services at ELFT working to optimise flow by using a systematic approach to addressing their backlogs, waiting times and increased demand. Staff and service users worked together across the whole healthcare system, including from GP referrals, primary care, community, and inpatient care.
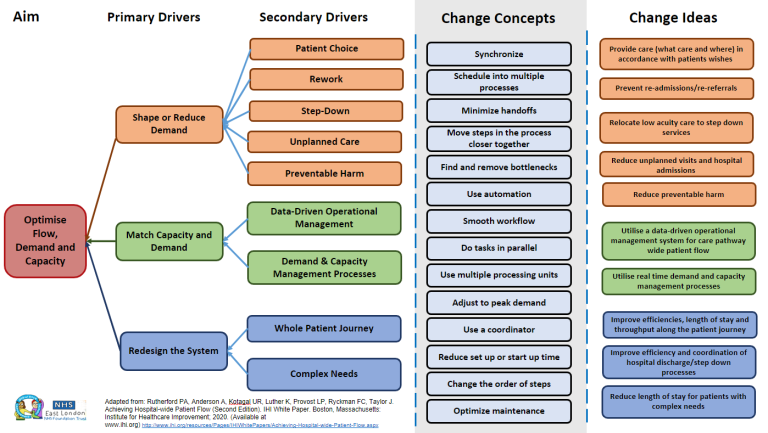
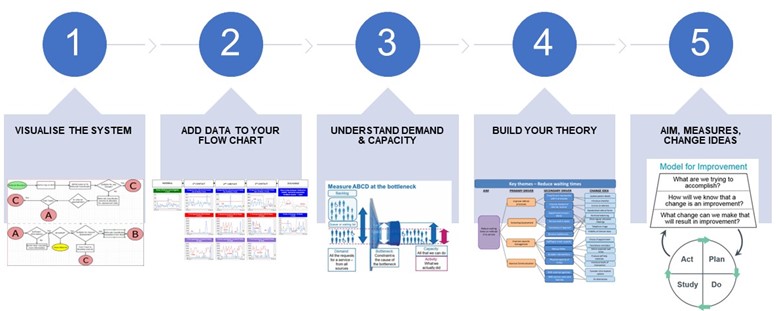
See below for our approach to optimising flow across the teams on the programme:
Throughout the programme, several change ideas were tested with notable improvements:
- Tower Hamlets Psychological Therapies: By eliminating duplication and redesigning their pathway, including reducing appointment calls, the time from referral to second contact dropped to under 12 weeks
- East London Community Eating Disorders Service for Children and Young People: Repurposing roles and having one senior clinician assess service users reduced average waiting times from 17 weeks to 5.4 weeks and decreased variation
- Newham CAMHS: An allocations spreadsheet was developed to manage a 30% increase in demand due to COVID-19, resulting in a 34% reduction in young people waiting for their first appointment
- Tower Hamlets Autism Service: The introduction of the “THAS pack” streamlined the referral process, reducing the time from referral to waiting list placement by 38%, saving around 12 days on average and easing administrative burdens
- Tower Hamlets Extended Primary Care: By having administrative staff handle booking and correspondence, clinical capacity increased, leading to a downward trend in people waiting for an initial occupational therapy assessment
Phase 4
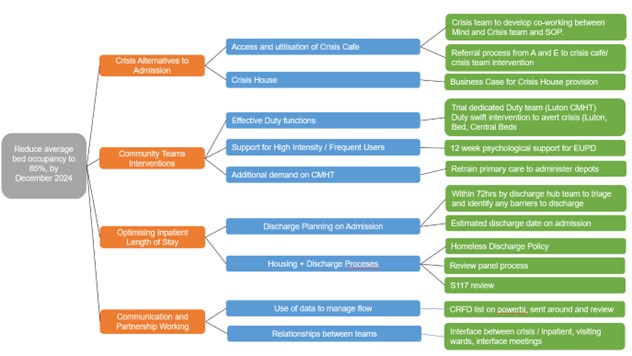
Phase four of the programme begun in April 2024 and is taking a whole systems approach to optimising flow, including community, inpatient and crisis services across Bedfordshire & Luton, City & Hackney, Forensic Services, Newham and Tower Hamlets.
The focus of the programme is as follows:
- To eliminate private bed usage by October 2024
- To reduce length of stay to 40 days by April 2025
- To reduce bed occupancy to 85%
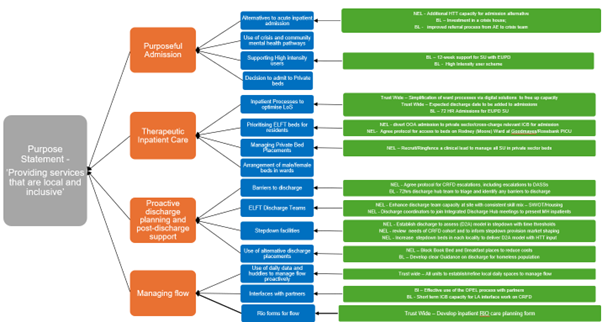
With a clear theory of change (see below) and collaborative efforts across our services, the Flow Programme is set to enhance and streamline patient care and maximise the use of our resources by ensuring our clinical teams can work at their highest levels of productivity and efficiency.
Related Stories
-
A collaborative approach to reducing inpatient bed occupancy in Bedfordshire & Luton
7th February 2024
-

-
End Of Flow QI Programme Summary
30th May 2023
Follow QI on social media
To keep up to date on the latest concerning QI at ELFT, follow us on our socials.