Adult Autism Service (Bedfordshire) – Our Improvement Journey

By Bedfordshire Adult Autism Service, Pat Moyce (Service User) and Mack Mclean (Carer)
Supported by Satwinder Kaur (QI Coach with Lived Experience)
The Adult Autism Service (Bedfordshire), aimed to reduce, in 7 months’ time, the average waiting times for first appointments from 59 weeks to 49 weeks by 31 January 2022
We commenced the project in June 2021 and followed the East London NHS Foundation Trust (ELFT) Sequence of Improvement and the Institute Healthcare Improvement (IHI) model for improvement to guide, structure and inform our improvement work. Our story is a combination of voices of staff, service users/carers and quantitative data.

Identification of a Quality Issue
The project focused on reducing average waiting times for patients referred to an assessment in the Bedfordshire Autism Service, in order to improve patient outcomes and staff experience. It is important to note there were external factors, such as the Covid-19 pandemic, which unveiled inequalities for those with complex needs in terms of access to services. These challenges also created opportunities for the autism team to use virtual platforms for assessments. Initially, this worked for many that had been referred to the service. However, overall waiting times for some had exceeded a year. The autism team decided to use the QI framework to solve this most complex problem, which was impacting on staff well-being and capacity to deliver outstanding quality care to all patients throughout the service.

Understanding the Problem: Voices of QI Project Team Members
“This QI project highlights that there are insurmountable limitations in capacity, and that, with further resources, the autism service could function in an even more efficient way. Working as a team, with those working at the Autism Service, and with Satwinder as QI coach, has enabled me to discover more about how QI functions to improve services, too.” (Mack Mclean Carer – QI Project Team member)
The QI Project team recognised patients had experienced digital exclusion on two levels:
- Limited access to technology
- The anxiety of dealing with communication that is outside the comfort of face-to-face conversations.
“I’m the Operational Lead for the Autism Service and have been the lead for the QI project, coordinating and placing specific responsibilities with individual colleagues. In order to engage service users effectively, I had to meet with service users outside of the main group meetings, as some of them do not cope well with being on screen.”
QI tools such as process mapping and the cause and effect diagram were used to understand the problem further during project team meetings.

Developing a Strategy and Change Ideas
Having fully understood the problem, the QI Project team developed a strategy (Figure 1) and change ideas to tackle the long waiting times.
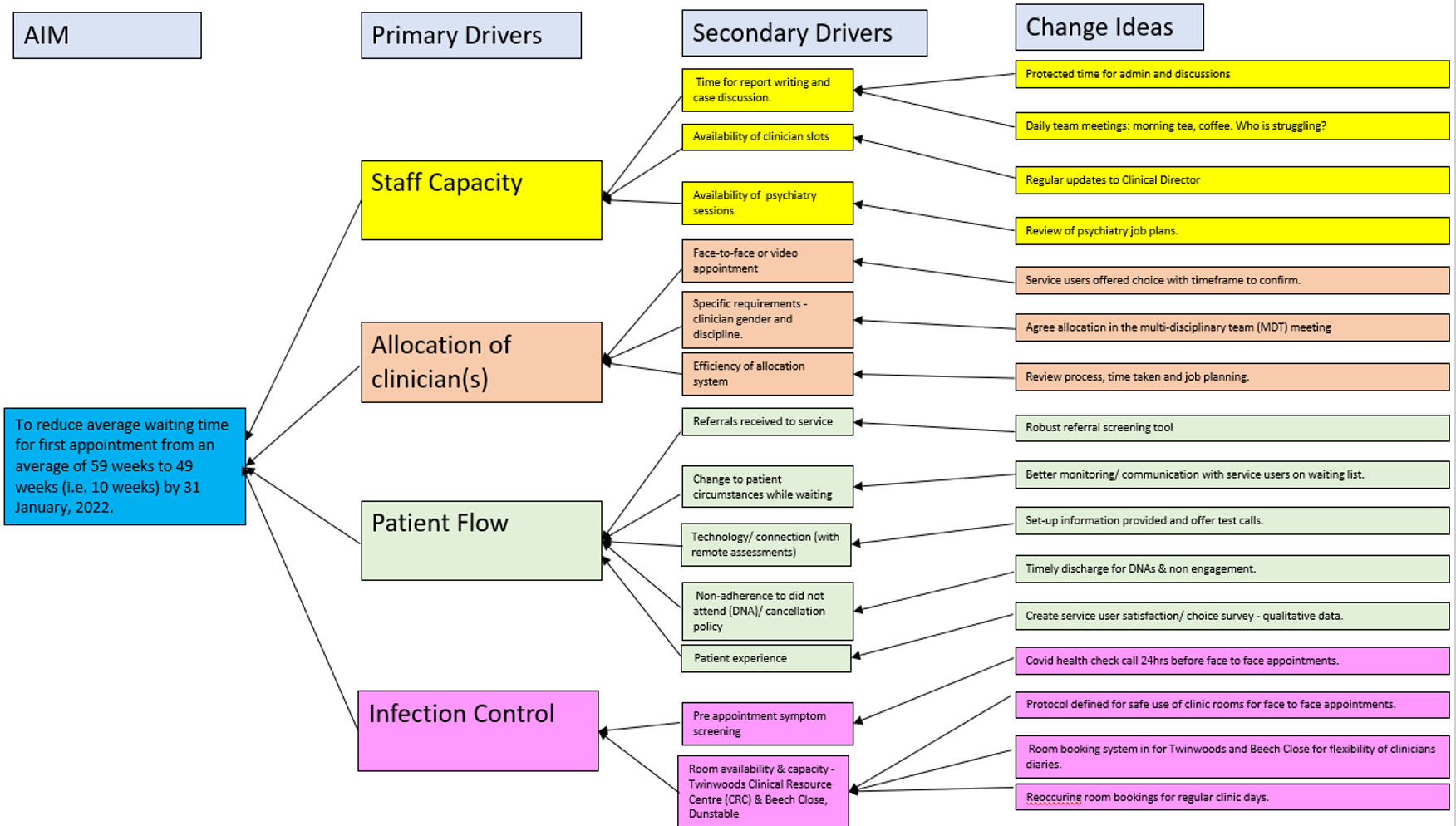
Figure 1: Strategy and change ideas developed by the Autism Service Bedfordshire team to reduce average waiting times in weeks for stage 1 assessments

Testing of Change Ideas: our reflections and learning
The team quickly moved to testing ideas to learn from the change ideas proposed by all. Below are comments from team members about what they learned.
Staff Capacity
- Protected time for administration and discussions – “This is mainly an issue for me & doctors. We do allocate time in calendars for discussions, so that’s business as usual. Protecting time for administration purposes is sorted for locum psychologists as part of job plan. As part of testing the idea of protected time for administration, I have negotiated a plan with the one psychiatrist; we have to protect one session per week for report writing. I have dedicated time each week for admin but sometimes it’s difficult to protect time because of other demands.” (Colin Parsons, Project Lead)
- Daily team meetings – “Not achieved, but we do have a weekly huddle in diaries and all chat or email on an almost daily basis.” (Colin Parsons, Project Lead)
- Updates to Clinical Director (CD) – “Not achieved. CD has moved to a different job in East London, so no direct oversight of service, although is still officially our CD. I am meeting with new line management instead regularly.” (Colin Parsons, Project Lead)
- Psychiatry job plans – “Not achieved. That was under discussion with CD & another Consultant Psychiatrist but did not progress. Since New Year (2022) they have both gone to jobs in East London (the Consultant Psychiatrist move is permanent, so the role for the Autism Assessment Service as Psychiatric Lead is vacant)” (Colin Parsons, Project Lead)
“Overall, we have lost staff capacity significantly, particularly with regards to psychiatry sessions. In addition, another staff member is leaving in April 2022 to do a one-year secondment in the Perinatal Team, that is another vacancy in the team.” (Colin Parsons, Project Lead)
Allocation of clinicians
1.Face-to-face or video appointment – this is now business as usual. All new accepted referrals are given option of how to engage, with a date by which to respond (and we send reminders). If no response, we assume option is face-to-face, but we update on waiting list if service user clarifies choice at any stage.
2.Specific requirements regarding staff profile – not achievable due to limited staff resources. If specific staff, such as a specified gender, is evidently appropriate or requested we will discuss through the multi-disciplinary team (MDT) & do our best to accommodate. We can be flexible, for example, if extra staff are needed to chaperone.
- Efficiency of allocation system – partially achieved during project. System has worked well in terms of allocating me or another staff member for stage 2 assessments, depending on our capacity, clinical needs, and our job plans/calendars define availability. Allocation to doctors for stage 1 assessments was governed by option for face-to-face (allocated to psychiatry) or video call (allocated to Locum Psychologist, as she only works remotely).
Patient Flow
- Referrals received to service – this is now business as usual. We have robust referral screening process in use and are tracking referrals accepted/declined via MDT meeting action log and on spreadsheet.
- Better monitoring/communication with service users on waiting list – not achieved. We still rely on contact from service users or other services working with them, rather than being able to do routine/proactive welfare checks.
- Tech/Connection (remote assessments) – this is now business as usual. Information sheet is sent out to people who have confirmed video call appointments, which includes offer to do test call if they want this. We will also offer test call if service user makes contact at any stage with concerns about process/set-up.
- Non-adherence to Did Not Attend (DNA)/cancellation policy – partially achieved. DNAs and cases outside “opt-in” deadlines are flagged through weekly MDT meeting action log. Main issue is staff capacity to follow these through for discharge in timely manner – can be a bit of a lag, but the process is working. PREM survey has been sent out and responses coming back – they need to be collated.
Infection Control
- Pre appointment screening – this is now business as usual. We have defined protocol for contacting people each week for upcoming appointments to ensure they are healthy/Covid-free and use of rooms. Guidance has been revised as national and Trust guidance has evolved.
- Room availability – this is now business as usual. Room booking system is in place & works well for both Twinwoods and Dunstable sites. There is work ongoing at Twinwoods to move some staff to create more room capacity for clinical appointments too. We do have recurring room bookings for regular clinic days to slot appointments into.

Measurement: Our Learning
Quality Improvement is about teamwork! Senior Clinical Support Workers with the Adult Autism Service: Rosie Deverick, described her role as: “Involved in creating and uploading all the information for the diagram on to the Life QI project online.”
Katrina Tibbetts said: “I have collated all the data, updated QI run charts, and scheduled all appointments for the clinicians, sometimes getting in touch with patients.”
Results: Our Learning
Although our QI project was aiming for an average reduction in waiting time of 10 weeks, this project achieved an average reduction of 28 weeks for patients waiting for a stage 1 assessment (15% reduction – Figure 2). This was a positive result for both staff and patients.
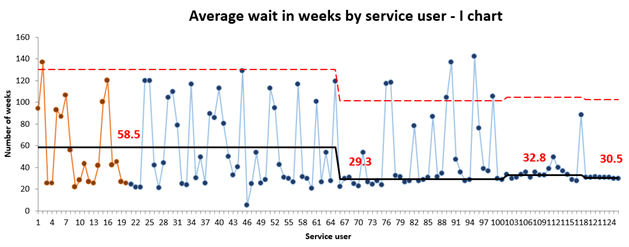
Figure 2: Waiting Time for a Stage 1 assessment (weeks) – I Chart
The team continues to monitor the quality of referrals coming through the service by plotting the data on relevant charts. They use this to understand and reduce variation and inform their practice and decision making. For example, they studied the percentage of referrals that were accepted each week. (Figure 3).
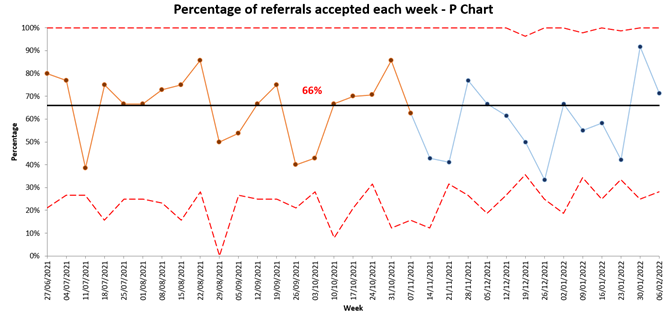
Figure 3: Percentage of referrals accepted each week (Process measure) – P Chart
Although the team has embraced and embedded QI in its daily practice, as is evident from the change ideas and data, there is a clear need within the system for more staff to be recruited as this team has lost the only two psychiatrists.
The rigour in practice of QI and rapidly embedding changes that improve the lives of those that are referred to this service demonstrates excellence in care.

Reflections from other QI Project Team Members
I am honoured to listen to people’s life stories… I complete assessments and short-term interventions focused on how someone manages to do activities important to their responsibilities, wellbeing, personal goals, and identity. (Erica Morrison, Senior Occupational Therapist)
It is essential, we think, to acknowledge the amount of work, and the different methodologies/change ideas that they have been applied to try to shorten the waiting times. Where there has been success, there has doubtless been improved outcomes for people with an autism spectrum difference. (Mack Mclean, Carer)
There is no failure in QI, this QI project team demonstrated a passion and commitment towards reducing their waiting times and using QI as the way to solve their most complex problem. I am truly privileged to have witnessed this dedication to QI by all the QI project team members. (Daisy Maradzika, Improvement Advisor)

The Amazing Autism QI Project Team: Bedfordshire
Colin Parsons: Project Lead
Erica Morrison: Senior Occupational Therapist
Rosie Deverick and Katrina Tibbetts: Senior Clinical Support Workers
Pat Moyce and Mack Mclean: Patient and Carer Team Members
Dr Sanjay Nelson: Project Sponsor and Directorate Clinical Lead for Learning Difficulties Service
Dr Imran Shakeel: Lead Psychiatrist in Autism Service Bedfordshire and Luton
Satwinder Kaur: QI Coach with Lived Experience
Daisy Maradzika: Improvement Advisor