Pursuing Equity
What is health equity?
Equity is one of the core aims of improving quality (2021, Institute of Medicine).
Equity in healthcare is described as “Absence of unfair, avoidable or remediable differences among groups of people, whether those groups are defined socially, economically, demographically, or geographically or by other dimensions of inequality.”
(World Health Organisation)
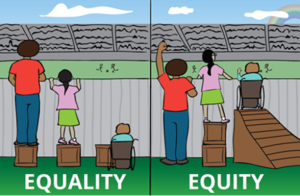
Equity differs from equality, which sees everyone treated the same irrespective of their circumstances. You can see this difference in the illustration.
Featured Article
Supporting teams to pursue equity
In response to the trust strategy to improve quality of life for all we serve, the trust has launched a Quality Improvement (QI) programme to support teams to pursue equity.
Phase one
The programme began in April 2022 and was designed in partnership with colleagues from public health, people participation, the trust’s networks, and the QI department.
The programme brought together 14 teams from across the trust, to support them to use QI to improve equity in their local areas. Topics that were tackled included
Across the programme 71% of teams tested at least one change idea and over 20 change ideas were tested in total, including but not limited to:
- Staff training around race
- Offering self-bookings, drop-in clinics and weekend appointments
- Women’s groups to talk about sexual issues on forensic inpatient wards
- Family interventions
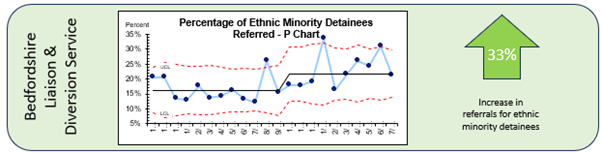
- Promoting services via barbers, gyms and social media to increase referrals from minority groups
- Redesigning clinical systems such as RiO to include screening status
- Recruitment videos
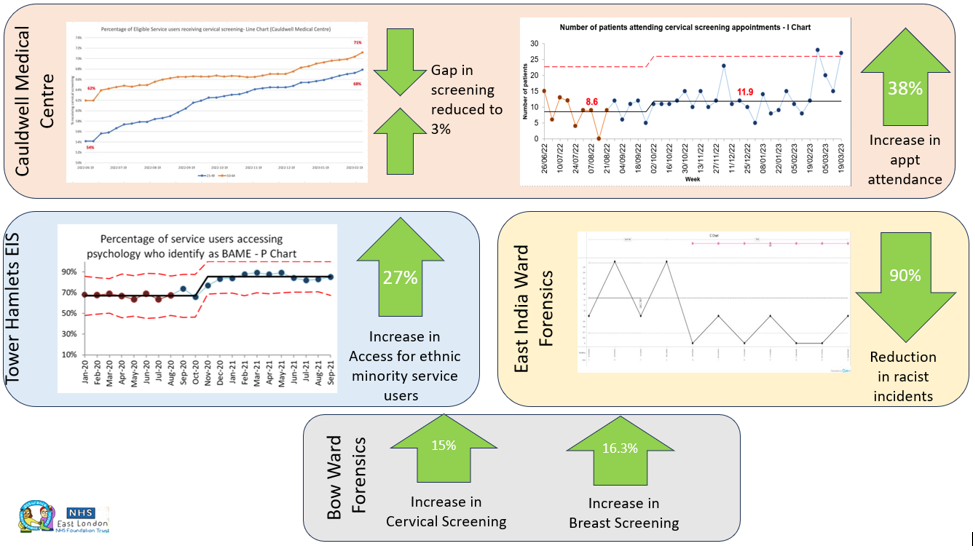
These change ideas resulted in 30% of teams seeing an improvement in their outcome measure, with 15% of teams also seeing an improvement in one of their process measures. See below for some of our most impactful results.
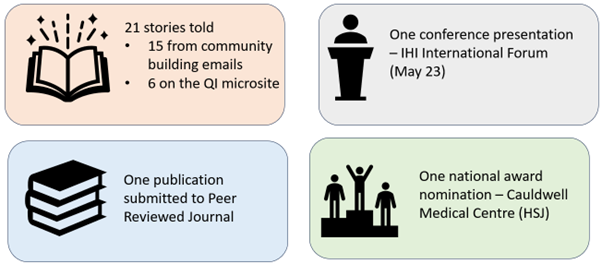
The wider impact of the work reached far and wide, including:
Phase two
The second phase of the programme began in September 2023 and built on the success of phase one to support teams to use QI to tackle inequity.
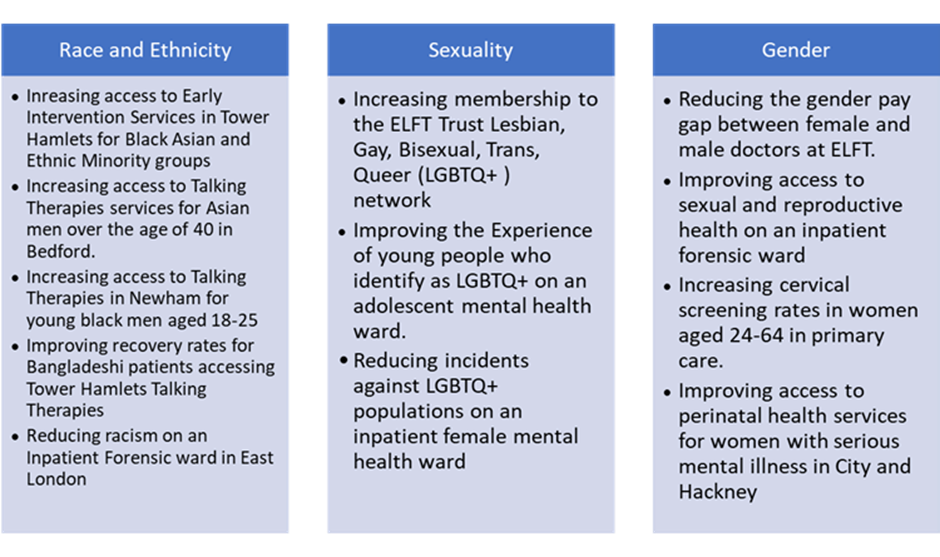
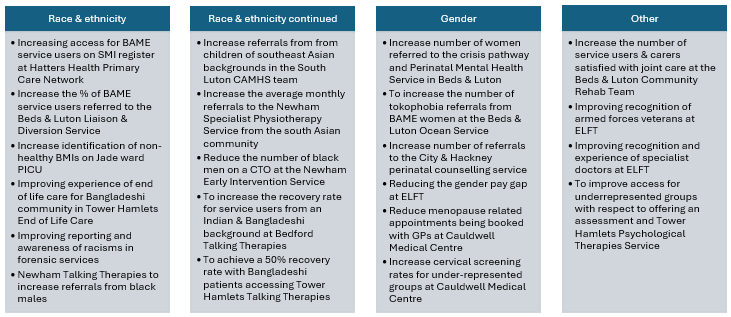
21 teams came together and used QI methods to tackle a wide range of equity issues that were most important to the teams and the populations they serve. Some examples of the work included:
Across the programme over 22 change ideas were tested. These ideas included:
- Running cross service / organisation meetings to inform clinical cases
- Training awareness so other teams understood the purpose of a service
- Translated information and treatment materials
- A podcast to inform people about services
- Clear processes for reporting racism
- Adjusting opt in processes to make it more accessible to certain demographic groups
- Doing home visits to people who could not attend the clinic
- Sharing care plans across services
- Animated information video (click here to view)
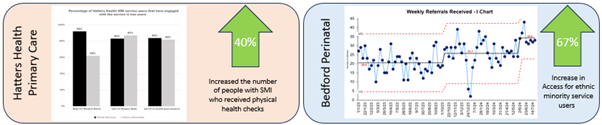
The impact of the work was far reaching, with three teams presenting their work at international conferences. Two teams were awarded prizes for their work and four peer reviewed publications have been published or are being currently written about the work. In addition to this, several teams on the programme saw an improvement in their outcome measure, including:
Phase three
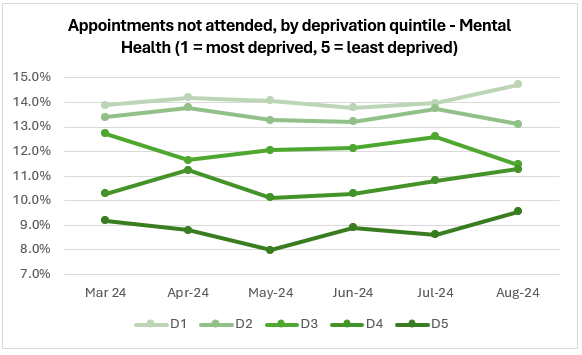
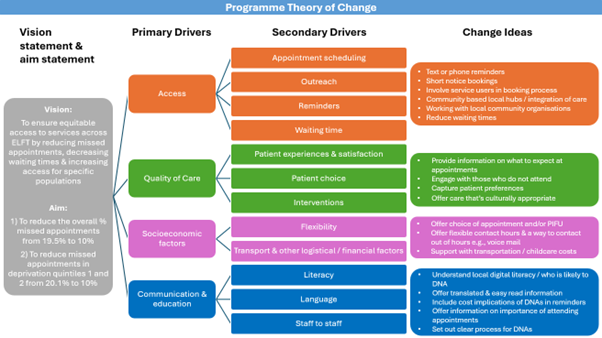
The third phase of the programme began in September 2024. This programme will address a Trust wide issue that shows people who live in the most deprived neighbourhoods are around 36% more likely to miss their appointments than those from our least deprived neighbourhoods.
The programme has brought together 31 teams from across ELFT and offered the chance to unite service users and staff from adult and older adult mental health, community health, specialist services, primary care and child and adolescent mental health services to reduce their missed appointments and tackle these inequities head-on.
With the support of QI, Data & Analytics, Population Health, and People Participation, teams will collaborate, innovate, and test ideas to create more equitable healthcare and a more productive and efficient service for all. Together, we aim to close the gap, reduce the waste of missed appointments, and ensure that no one’s health is left behind.
See below for the programme theory of change:
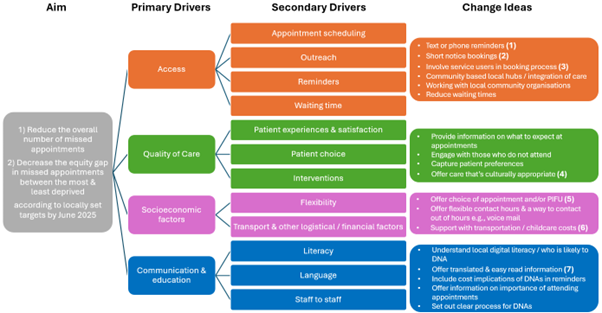
The programme offers comprehensive support to help teams succeed:
Monthly learning sessions: Teams participate in 50-minute sessions to share insights, learn from one another, and plan their next steps in reducing missed appointments.
Change idea menu: Teams have access to a practical menu of evidence-based change ideas, designed to help reduce missed appointments and drive improvements. To view this document, click here.
Digital improvements: Work is underway with the Trust’s Digital team to enhance communication with patients and improve both staff and patient experiences around appointments.
Poverty-focused tools: We’ve partnered with Population Health and a Poverty Proofing charity to introduce tools that help tackle poverty in our most deprived communities.
Data tracking and insights: We’re working with the Data and Analytics department to provide teams with fortnightly data reports and a PowerBI dashboard helps track missed appointments by deprivation, gender, ethnicity, age, and sexual orientation.
Related Stories
-
-

-
Breaking Down Barriers: Young People Tackling Inequity Through Quality Improvement Projects
17th February 2025

Follow QI on social media
To keep up to date on the latest concerning QI at ELFT, follow us on our socials.